Inflammatory bowel disease (IBD), which include Crohn’s disease and ulcerative colitis, affect as many as five million people worldwide. The main difference between the two diseases is the parts of the digestive tract they affect. In Crohn’s disease, inflammation can affect any part of the gastrointestinal (GI) tract from the mouth to anus while ulcerative colitis affects the colon and the rectum.
Another type of inflammatory bowel disease is indeterminate colitis, in which features of both the diseases are present and when it is difficult to distinguish between them. Rarer forms of IBD are two main types of microscopic colitis - collagenous colitis and lymphocytic colitis.
The factors that cause IBD are unknown, but several probable risk factors have been studied. Some of them are:
Since the symptoms of IBD vary from person to person, doctors have a hard time diagnosing what kind of IBD a patient might have. Patients may also experience long periods of remission when the disease is not active and recurrent flare-ups. Complications of IBD include:
IBD can also have extra intestinal issues such as:
To diagnose IBD, your doctor will take your history and perform a physical exam, which may then be followed by one or more tests such as:
Blood tests can find signs of anemia or to check for signs of infection from bacteria or viruses while stool tests identify intestinal inflammation. Blood tests may also assess liver and kidney functions, which can be affected by IBD.
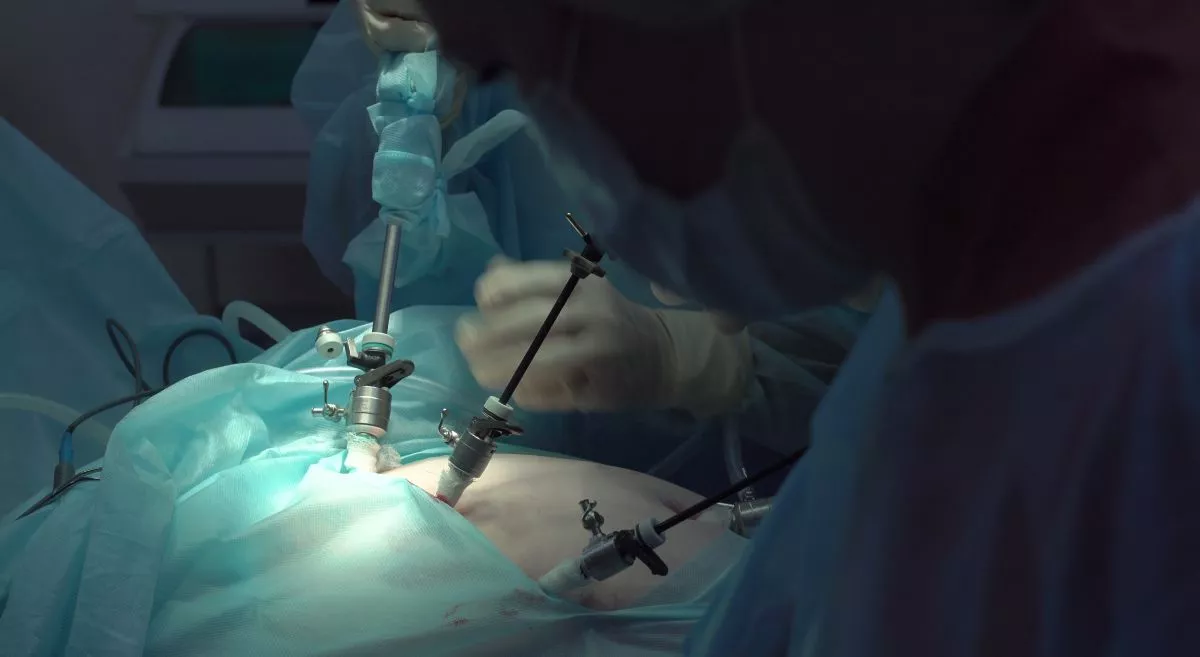
This method lets your doctor look inside your body using an endoscope which has a tiny camera attached to it. It helps your doctor to see if inflammation is present, where it is located, assess its severity, and obtain biopsies to confirm the diagnosis.
This is the type of endoscopy most often performed to both diagnose and monitor IBD. This test allows your doctor to view your entire colon. During the procedure, your doctor can also take a biopsy to confirm a diagnosis.
This test is an endoscopic evaluation of the sigmoid colon and to confirm the presence of inflammation in that part of the colon. The procedure uses a camera, which is inserted through the anus to look for ulcers, fistulas, and other damage.
This is an examination of the small intestine which uses a special type of endoscope with two small balloons at its tip. It can be used to examine and take biopsies from the whole length of the small intestine.
This process allows your physician to obtain pictures of the entire small bowel. For the test, you swallow a small capsule containing a camera, which then passes through the small intestine and transmits images to a data recorder worn around the waist. The capsule is then excreted in the stool normally.
This is a relatively new technique that uses a special type of endoscope that has a tiny ultrasound transmitter at its tip. The scope is then passed through the mouth or anus to the area to be examined. This process produces very clear, detailed images of the digestive tract.
CT scans are basically computerized X-rays that looks at the entire bowel as well as at tissues outside the bowel. The CT scan is used to detect complications of IBD, such as intra-abdominal abscesses, strictures, small bowel obstructions or blockages, fistulas, and bowel perforation.
MRI uses magnetic fields and radio waves to create detailed images of the body and is especially helpful in examining soft tissues and detecting fistulas. There is also no radiation exposure with MRI.
There are several different medications to treat IBD, but if medical treatment is ineffective, then bowel resections, strictureplasties, colostomy or ileostomy may be necessary. The most commonly prescribed medications for IBD fall into five classes. They are:
Who is at risk of getting IBD?
Genetics -
There is clearly a genetic factor for getting the disease. Studies have shown that 5% to 20% of affected individuals have a first-degree relative, either a parent, child or sibling with one of the diseases. The risk is also substantially higher when both parents have IBD.
Smoking -
Smokers are more likely to get Crohn’s disease and it can increase the risk of complications. However, smokers are at lower risk of developing ulcerative colitis.
Age -
Although IBD can happen at any age, people are often diagnosed between the ages of 15 and 35. About 10% of cases occur in individuals less than 18 years old.
Gender:
IBD affects both women and men, but more often in women, possibly due to certain hormones.
Geographic distribution:
IBD is found mostly in developed countries and among people who live in urban areas.
What are the symptoms of IBD?
Urgency to have a bowel movement
Bloody stools
Anemia
Diarrhea
Abdominal pain
Rectal bleeding
Extreme fatigue
Nausea and vomiting
Eyes redness, pain, and itchiness
Mouth sores
Arthritis
Skin disorders
Osteoporosis
Kidney stones
Depression
How is IDB diagnosed?
Blood and stool tests –
Endoscopy –
Colonoscopy -
Flexible Sigmoidoscopy -
Double Balloon Enteroscopy (DBE) -
Capsule Endoscopy –
Endoscopic Ultrasound (EUS) -
Computer Tomography (CT) -
Magnetic Resonance Imaging (MRI) –
What are the treatment options for IBD?
Aminosalicylates -These drugs, which contain 5-aminosalicylic acid (5-ASA), decreases the inflammation of the digestive tract and in preventing relapses. They can be given either orally or rectally. Examples are sulfasalazine, balsalazide, mesalamine, and olsalazine.
Corticosteroids -These medications, which include prednisone, prednisolone, and budesonide keep the immune system in check and are effective for short-term control of flare-ups.
Immunomodulators -This group of medication can be given orally or by injection. They prevent the immune system from attacking the bowel and causing inflammation. Examples of immunomodulators are azathioprine, cyclosporine, 6-mercaptopurine, and methotrexate.
Biologic therapies -These are the latest drugs developed to treat IBD and are effective in achieving and maintaining remission without the use of steroids. They help to reduce inflammation by targeting specific proteins that play a role in inflammation. There are two main classes of biologics. The first are the Anti-tumor necrosis factor (anti-TNF) agents such as adalimumab, certolizumab pegol, golimumab, infliximab, and infliximab-dyyb while the second categories are the anti-integrins such as natalizumab and vedolizumab.
Antibiotics -Given orally or intravenously, antibiotics such as metronidazole and ciprofloxacin are used to kill bacteria that may trigger or aggravate IBD symptoms.
Over the last decade, major advancements, specifically in the fields of genetics, immunology, and microbiology, and the development of increasingly effective treatments have led to a greater understanding of inflammatory diseases of the digestive system. These key breakthroughs have also helped to transform treatment for the many patients who suffer from IBD.
Featured Blogs
One Aster
Personalized Medical Assistant for all your healthcare needs.
Book instant appointment, pay securely, eConsult with our doctors and save all your health records at one place are some of the benefits of OneAster App. It is everything you need, to manage your family Health.
* Registration available only for valid Indian mobile number