The Aster Centre of Excellence (CoE) in Neurosciences at Aster Whitefield Hospital stands as a beacon of advanced healthcare, offering comprehensive services in neurology, neurosurgery, spine surgery, neuro-oncology, neuroradiology, neuropsychology, and neurorehabilitation for patients of all age groups. Renowned as one of the premier Neurological Hospitals, the Centre of Excellence in Neurosciences at Aster Whitefield is committed to delivering specialized treatment and care for a broad spectrum of conditions impacting the brain, spinal cord, and peripheral nervous system.
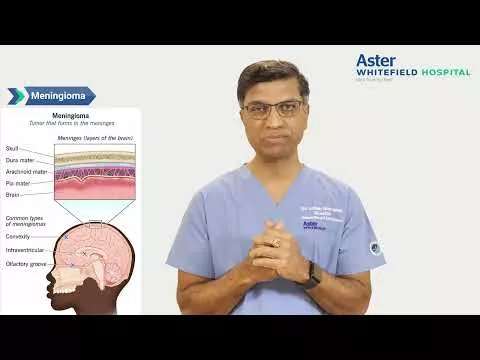
The department excels in administering major neurosurgical treatments, encompassing Movement Disorders, Vascular and Endovascular Neurosurgery, Brain Tumor Surgery, Aneurysm, AVM Surgeries, Interventional procedures, Pediatric Neurosurgery, Epilepsy Surgery, Deep Brain Stimulation, Stroke Care, Neuro Rehabilitation Care, and Chronic Pain. Additionally, it focuses on spinal treatments for spinal tumors, disc herniation, cervical/lumbar spondylosis, sciatica, and congenital spinal deformities.
Our exceptional team of doctors consists of nationally and internationally trained neurologists, neurosurgeons, spine surgeons, neuroradiologists, and neuropsychologists, adept at handling the most complex cases. With a multidisciplinary approach, they ensure optimal and evidence-based treatment, supported by specialty-trained nurses, technicians, and rehabilitation therapists.
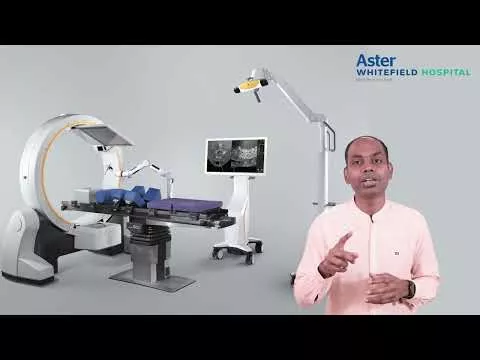
Advanced Technology & Facilities
Well equipped with the latest medical equipment, modern technology & infrastructure, Aster Hospital is one of the best hospitals in India.
Aster Whitefield Hospital's Epilepsy Comprehensive Program is a program where expertise meets compassion in the pursuit of managing and treating epilepsy. Our program is dedicated to providing holistic care, employing cutting-edge technologies and a multidisciplinary approach to improve the lives of individuals affected by epilepsy.
Epilepsy, a neurological disorder characterized by recurrent seizures, demands specialized attention and tailored treatment strategies. At Aster Whitefield Hospital, we understand the challenges faced by individuals with epilepsy and their families. Our team of renowned neurologists, neurosurgeons, and healthcare professionals collaborates seamlessly to offer personalized care and innovative solutions.
Our commitment to excellence extends to the forefront of epilepsy care, integrating advanced diagnostics, precise surgical interventions, and comprehensive follow-up care. We believe in empowering our patients through education, support, and access to the latest advancements in epilepsy management.
With a focus on individualized treatment plans, our program strives to enhance the quality of life for each patient. We prioritize patient comfort, safety, and successful outcomes throughout their journey with us.
Visit us to explore our range of specialized facilities, each designed to provide accurate diagnoses, targeted interventions, and ongoing support for patients.
- VideoElectroencephalogram (VEEG):
A Video EEG (VEEG) is a non-invasive diagnostic test that combines video recording with electroencephalography (EEG) to monitor brain activity. This specialized test is instrumental in identifying various seizure types and evaluating the effectiveness of treatments. It allows for the simultaneous observation of brainwave activity during a seizure or spell, aiding in determining its nature and guiding tailored treatment approaches.
This test, requiring hospital admission, typically spans three to five days. Its primary purpose is to diagnose episodic events that occur intermittently, such as epileptic seizures, blackout spells, unexplained episodes, confusion, hallucinations, or behavioral issues.
By capturing brain activity during both normal and seizure episodes, a VEEG assists in precisely correlating changes in behavior with specific EEG patterns. This correlation is pivotal in providing a more accurate diagnosis and understanding of the underlying neurological condition. The information gleaned from a VEEG not only helps in characterizing the nature of seizures or spells but also aids healthcare providers in devising the most effective treatment strategies tailored to the individual's needs.
Our expert team utilizes state-of-the-art equipment to conduct continuous monitoring, ensuring accurate results crucial for personalized treatment plans.
- Electrocorticography (EcoG):
Electrocorticography (ECoG) involves placing electrodes directly on the brain's surface to monitor its electrical activity, often used during surgery to locate the origin of seizures. In contrast, ElectroCochleoGraphy (ECoG) is a diagnostic test used in Meniere’s disease and related conditions, measuring electrical responses in the inner ear to sound stimulation.
During an ECoG test, a sticker electrode is placed on the forehead, and foil-covered earphones are gently inserted into the ear canals after cleansing. An audio stimulus is then delivered through the earphones, eliciting cochlear activity, which is recorded by an electrode. Once the measurements are obtained, the electrodes and earphones are removed, allowing the patient to resume their usual activities.
In surgical settings, ECoG is performed by skilled neurosurgeons to pinpoint seizure sources and assess suitability for resective surgery. This technique offers high-resolution brain monitoring, enabling real-time mapping of brain function. This precise mapping enhances surgical accuracy, minimizing the impact on healthy brain regions.
- Stereo EEG (SEEG):
SEEG, or Stereoelectroencephalography, is a minimally invasive procedure utilizing advanced technology to implant electrodes through small skull openings into the brain tissue. These electrodes monitor and precisely identify the origin of seizures in children. By reaching deeper and more extensive brain areas compared to a standard EEG, SEEG allows neurosurgeons to pinpoint where challenging-to-treat epileptic seizures start.
This sophisticated technique involves implanting up to 20 electrodes, each about 0.8mm in diameter—similar to the width of spaghetti strands—into the brain tissue through tiny skull holes. These electrodes facilitate monitoring and precise identification of seizure onset zones, aiding in treatment decisions.
Our hospital provides advanced Stereo EEG procedures focused on accurately locating seizure origins. This minimally invasive approach ensures precise electrode placement, enabling comprehensive mapping of seizure networks within the brain. SEEG plays a crucial role in complex cases, guiding clinicians in treatment planning and significantly improving surgical outcomes.
- Vagus Nerve Stimulation (VNS):
Vagus Nerve Stimulation (VNS) is a surgical implant designed to send mild electrical impulses to the brain through the vagus nerve, diminishing both the frequency and severity of seizures. FDA-approved as an additional therapy for individuals aged 4 and above with drug-resistant or refractory epilepsy, VNS Therapy® aims to alleviate focal or partial seizures that remain uncontrolled by medications.
The therapy involves a device implanted beneath the skin in the left chest area, connected to an electrode wrapped around the vagus nerve in the neck. This device, programmable in outpatient clinics, administers regular pulses of stimulation without requiring any action from the patient. Generally, individuals are unaware of the stimulation process.
If individuals sense an impending seizure, swiping a magnet over the implanted generator can trigger an extra burst of stimulation, potentially aiding in seizure cessation. VNS, a form of neuromodulation, aims to alter brain cell activity by providing targeted electrical stimulation to seizure-involved areas.
Our specialized team excels in VNS implantation, offering a proven therapy for managing epilepsy. This programmable device delivers controlled electrical pulses to the brain, providing substantial seizure reduction for patients who have not responded to conventional medications or other treatments.
Aster Whitefield Hospital's Stroke Comprehensive Program is dedicated to providing exceptional care and comprehensive solutions for individuals affected by strokes. Our program embodies a multidisciplinary approach, combining expertise, innovation, and compassion to address the complexities of stroke care
- Thrombolysis
Thrombolysis is a vital medical procedure involving the administration of clot-dissolving medications to address blockages within arteries during critical conditions like acute ischemic stroke. Also known as fibrinolytic therapy, this treatment plays a crucial role in restoring blood flow by dissolving dangerous intravascular clots and preventing ischemic damage.
It finds application in several conditions, notably ST-elevation myocardial infarction, stroke, and severe venous thromboembolism, including cases of massive pulmonary embolism or extensive deep vein thrombosis. In heart attacks, large-scale trials have demonstrated reduced mortality through thrombolysis, particularly fibrinolysis, which triggers secondary fibrinolysis by plasmin via tissue plasminogen activator (tPA) analogs.
For stroke patients within a certain time frame from onset and without contraindications, thrombolysis significantly reduces the risk of major disability or death. Additionally, in instances of massive pulmonary embolism or severe deep vein thrombosis threatening limb loss, catheter-directed therapy or intravenous thrombolysis provides effective alternatives.
Thrombolysis is commonly administered intravenously but can also be directed into affected blood vessels through techniques like intra-arterial thrombolysis during an angiogram. Medical experts across various specialties, including interventional radiologists, vascular surgeons, cardiologists, and neurosurgeons, perform this procedure. In certain countries, emergency medical technicians or practitioners under specific qualifications may initiate thrombolysis for heart attacks in prehospital settings, always after assessing risks and benefits against other available interventions.
Aster Whitefield Hospital stands out for its expertise in thrombolytic therapy, promptly administering clot-dissolving drugs following an ischemic stroke. This intervention focuses on dissolving clots, reinstating blood flow to the brain, and safeguarding crucial neurological functions.
- Mechanical Thrombectomy
Mechanical thrombectomy stands as a minimally invasive procedure aimed at clearing blood clots lodged within brain blood vessels following an ischemic stroke. This advanced endovascular technique involves a small incision in the groin, through which thin tubes (catheters) are delicately threaded into the vessels leading to the clot.
Primarily utilized for removing clots in the brain, heart, or lungs, mechanical thrombectomy plays a critical role in addressing ischemic stroke and myocardial infarction both significant global causes of mortality. The contemporary approach to managing these conditions encompasses intravascular thrombolytics, mechanical thrombectomy, or a combination thereof.
Key objectives of this procedure involve understanding its indications, comprehending the necessary equipment, the role of personnel, preparatory measures, and the precise technique involved. It also involves recognizing potential complications and their clinical significance, ensuring comprehensive management.
Mechanical thrombectomy employs various catheter-based therapies, predominantly stent-retrieval, direct aspiration, or a combination of both, guided by image-based precision to remove clots effectively.
Our hospital specializes in mechanical thrombectomy procedures. Our neuro-interventional team leverages specialized devices and expertise to meticulously extract clots, thereby restoring blood flow and potentially reversing severe stroke effects. Equipped with state-of-the-art imaging technology, we ensure the precise execution of these intricate procedures, aiming for optimal patient outcomes.
The Neurophysiology Program at Aster Whitefield Hospital is where cutting-edge technology meets expert care to provide a comprehensive array of services dedicated to diagnosing and treating neurological conditions. Our program is committed to delivering accurate assessments and personalized care, ensuring optimal outcomes for our patients.
- Electroencephalogram (EEG)
The electroencephalogram (EEG) serves as a non-invasive diagnostic test capturing brain activity by detecting variations in electrical patterns linked to neurological conditions. Through the placement of small sensors on the scalp, this painless procedure records the brain's electrical signals, which are then analyzed by a medical professional.
Using metal discs (electrodes) attached to the scalp, the EEG records the continuous electrical impulses exchanged by brain cells, even during sleep, visualizing this activity as wavy lines on the recording.
Primarily utilized as a key diagnostic tool for epilepsy, the EEG plays a vital role in identifying various brain disorders. It can detect alterations in brain activity, aiding in the diagnosis of epilepsy, seizure disorders, and a spectrum of other conditions.
The test's diagnostic capabilities extend to identifying brain tumors, damage resulting from head injuries, diverse causes of brain dysfunction (encephalopathy), sleep disorders, inflammation like herpes encephalitis, strokes, and conditions like Creutzfeldt-Jakob disease.
Our hospital integrates advanced EEG technology to meticulously monitor brain activity, facilitating the diagnosis of seizures, epilepsy, and an array of neurological disorders. Our adept team ensures precise recordings and in-depth analysis, enabling accurate diagnoses and tailored treatment plans for optimal patient care.
- Electroneuromyography (ENMG - Nerve Conduction Studies & Electromyography)
ENMG, or electromyoneurography, is a diagnostic method that combines electromyography and electroneurography to assess both nerve and muscle functions. By measuring a peripheral nerve's conduction velocity and recording muscular activity, this technique provides valuable insights into neuromuscular diseases, aiding in accurate diagnoses.
Using surface electrical probes, ENMG collects electrophysiological data from nerve and muscle cells. Surface electrodes capture nerve activity by stimulating the nerve at one point and recording from another, measuring the time it takes for the potential to travel between the sites to determine conduction velocity. Additionally, the potential amplitude serves as a gauge of the number of conducting fibers, with abnormalities such as low or absent amplitude signaling potential nerve damage.
At Aster Whitefield Hospital, our comprehensive ENMG assessments encompass nerve conduction studies and electromyography. These tests are instrumental in diagnosing various conditions, including peripheral neuropathies, radiculopathies, and muscle disorders. By evaluating nerve functionality and muscle health, these assessments contribute crucial information that guides accurate diagnoses and tailored treatment plans for patients.
- Visual Evoked Potential (VEP)
Visual Evoked Potential (VEP) testing is a non-invasive procedure crucial in diagnosing conditions impacting the coordinated function between the eyes and the brain in interpreting visual stimuli. By measuring the electrical signals generated by the brain's visual cortex in response to visual stimulation, VEP aids in detecting disorders affecting the optic nerve and visual pathway.
This test specifically assesses the functionality of various components within the visual pathway, including the eyes, optic nerves, optic chiasm, optic tract, optic radiation, and cerebral cortex. Any abnormalities affecting these components can manifest as irregularities in the VEP test results.
VEP testing plays a significant role in diagnosing a spectrum of conditions. It is particularly instrumental in identifying multiple sclerosis-related optic neuritis, gliomas on the optic nerve due to neurofibromatosis type 1, compression on optic pathways, traumatic head or brain injuries causing visual pathway damage, toxic optic neuropathy resulting from specific medications or toxins like carbon monoxide, and other types of optic neuropathies such as anterior ischemic optic neuropathy or those associated with infections like meningeal tuberculosis.
Additionally, VEP tests aid in monitoring the progression of certain neurodegenerative conditions like multiple sclerosis, Leber optic neuropathy, Kjer-type dominant optic neuritis, and Friedrich's ataxia.
During the test, electrodes are placed on specific areas of the scalp while the individual views a visual stimulus, commonly a flashing checkerboard pattern. These electrodes record the brain's electrical activity in response to the stimulus. The resulting wave patterns are interpreted by specialists to identify any abnormal activities, which could signify issues within the visual pathway.
Our hospital specializes in conducting VEP tests to evaluate the integrity of the visual pathway. This diagnostic tool serves as a cornerstone in identifying conditions affecting vision, such as optic neuritis, multiple sclerosis, and various neurological disorders impacting visual health.
- Somatosensory Evoked Potentials (SSEP)
SSEP, or Somatosensory Evoked Potentials, stands as a vital method for assessing nerve pathway functionality by recording responses to sensory stimuli. Particularly prevalent in spine surgery, SSEPs have emerged as a crucial neurophysiological monitoring tool due to their remarkable sensitivity and specificity in identifying spinal cord injuries. Their implementation has significantly reduced the occurrence of new postoperative neurological deficits.
Notably, SSEPs play a pivotal role in localizing regions within the nervous system. They demonstrate an ability to identify functional areas of the human cortex during brain surgery, showcasing their potential in assisting with surgical procedures. In cases of cervical or cervicomedullary spinal cord stimulation, SSEPs have proven effective in predicting the lateralization of an epidural electrode and the resulting stimulation-induced paresthesias, ensuring precision during procedures.
Continuous monitoring using SSEPs serves as a safeguard during surgical processes, alerting the surgical team to any unintended movement of electrodes during anchoring and closing stages. This real-time surveillance aids in maintaining the intended electrode position, enhancing procedural accuracy and patient safety.
At Aster Whitefield Hospital, SSEP assessments are routinely conducted to evaluate nerve pathways in various conditions. These assessments prove instrumental in diagnosing and monitoring spinal cord injuries, multiple sclerosis, and a spectrum of other neurological disorders impacting sensation. Through SSEP evaluations, our hospital ensures comprehensive assessment and tailored management strategies for patients with these conditions, prioritizing accurate diagnoses and optimized treatment outcomes.
- Brainstem Evoked Response Audiometry (BERA)
The Brainstem Evoked Response Audiometry (BERA) serves as an objective test assessing hearing by recording electrical brainstem responses to auditory stimuli, typically clicking noises directed into the ear. It evaluates the transmission of electrical waves from the eighth cranial nerve to the brainstem, examining the auditory system's electrical potential from the cochlea to the cortex.
BERA proves instrumental in diagnosing lesions in the VIII nerve and the auditory pathway in the brainstem, especially in adults. It stands out for its accuracy and sensitivity in differentiating between cochlear and retrocochlear hearing loss, offering a non-invasive, easily recordable, and cost-effective diagnostic method.
The test holds significant importance, particularly in early childhood, where hearing disorders or complete deafness occur in approximately 1 in 1000 children. Its efficacy lies in providing a swift and efficient screening method for deafness in infants, particularly useful when traditional audiometric tests may not be feasible. BERA stands as a vital objective tool for evaluating the peripheral auditory system in neonates, infants, sedated individuals, and those unable to communicate verbally.
Conducting BERA aids in determining the type, severity, and nature of hearing abnormalities, offering valuable insights into conductive or sensorimotor issues, hearing thresholds, and the site of hearing loss within the inner ear or other auditory structures.
Moreover, the test serves broader diagnostic purposes, assisting in identifying various conditions affecting hearing, such as nerve tumors, brain tumors, multiple sclerosis, and other nerve disorders.
The procedure involves the placement of electrodes on the scalp to record brainstem potentials in response to auditory stimuli, primarily click stimuli. BERA proves effective in screening newborns for deafness, intra-operative monitoring of the nervous system, and diagnosing suspected demyelinated disorders.
At our hospital, BERA tests play a crucial role in assessing hearing function, aiding in diagnosing hearing impairments and neurological conditions affecting the auditory pathways with precision and expertise.
- Botox Therapy
Botox therapy involves the use of botulinum toxin injections to address various neurological conditions that result in muscle spasticity or movement disorders. It has been effectively utilized in treating several neurologic disorders such as facial muscle blinking or twitching, dystonias, and spasticity stemming from strokes, multiple sclerosis, or brain injuries.
In the realm of neurology, Botox treatment acts by blocking nerve signals in specific areas, particularly the neck and forehead, to alleviate migraines. While it doesn't eliminate migraine triggers, Botox significantly reduces their intensity. The effects of one dose typically last for 10-12 weeks and, with repeated treatments, have shown a remarkable 50% reduction in migraine occurrences.
Notably, one of the most promising applications of botulinum toxin lies in managing chronic migraines. This treatment has brought relief to those who previously relied on over-the-counter pain relievers or other medications.
Furthermore, Botox therapy extends to managing spasticity in individuals with multiple sclerosis, cerebral palsy, brain trauma, or ALS. It has also proven effective in addressing conditions like hypersalivation associated with Parkinson's disease, ALS, or cerebral palsy. The precision of botulinum toxin injections, administered every few months, aids in regulating saliva production and managing involuntary muscle contractions, such as in cervical dystonia or eye twitching (blepharospasm).
Our specialized team focuses on administering Botox therapy for conditions such as spasticity, dystonia, and nerve-related pain syndromes. Through targeted injections, we aim to alleviate muscle stiffness and enhance functional abilities for individuals grappling with various neurological conditions.
In the realm of spine care, Aster Whitefield Hospital stands as a beacon of excellence, offering a comprehensive range of services designed to meet the diverse needs of patients worldwide. Our commitment to international expertise, cutting-edge technology, and academic excellence sets us apart as a leader in spine surgery.
At Aster Whitefield, we take pride in our truly international patient base, fostering cultural sensitivity and understanding of varied medical backgrounds. Our multilingual staff ensures seamless communication, providing a personalized experience. With world-class infrastructure equipped with advanced diagnostic tools, including MRI, CT, and EOS scans, we ensure accurate diagnoses. Our three dedicated operating rooms feature state-of-the-art technology for safe and efficient procedures, while specialized outpatient departments and a rehabilitation center offer comprehensive pre- and post-surgical care.
Our internationally renowned surgical team comprises experts trained at top global institutions. Possessing exceptional surgical skills, they actively contribute to academic research, staying at the forefront of advancements and ensuring excellent clinical outcomes.
Utilizing cutting-edge technologies like IONM, Leica Microscopes, Canon Biplane Spine Suite, and minimally invasive robotic surgery systems , Aster Whitefield ensures advanced and efficient care. Our multidisciplinary team collaborates seamlessly, including neuro anesthetists, pathologists, radiologists, oncologists, reconstructive surgeons, and rehabilitation professionals.
Our commitment to excellence extends to specialized paramedics ensuring safe spine care. Emphasizing preventive measures alongside treatment options, we provide comprehensive spine care covering the entire cervical to sacral region. Innovative technologies, such as 3D Virtual Reality, aid in patient education and informed decision-making.
Surgeons at Aster Whitefield are not just practitioners but contributors to the advancement of spine surgery. With over 100 articles published in leading spine journals, authored medical books, national and international conference presentations, and numerous awards, our surgeons lead the way in research, improving the diagnosis and treatment of spine disorders.
At Aster Whitefield Hospital, we redefine spine care through a combination of international expertise, cutting-edge technology, and a commitment to academic excellence. Your spine's well-being is our priority, and we strive to provide unparalleled care that makes a difference.
Blogs
The source of trustworthy health and medical information. Through this section, we provide research-based health information, and all that is happening in Aster Hospital.