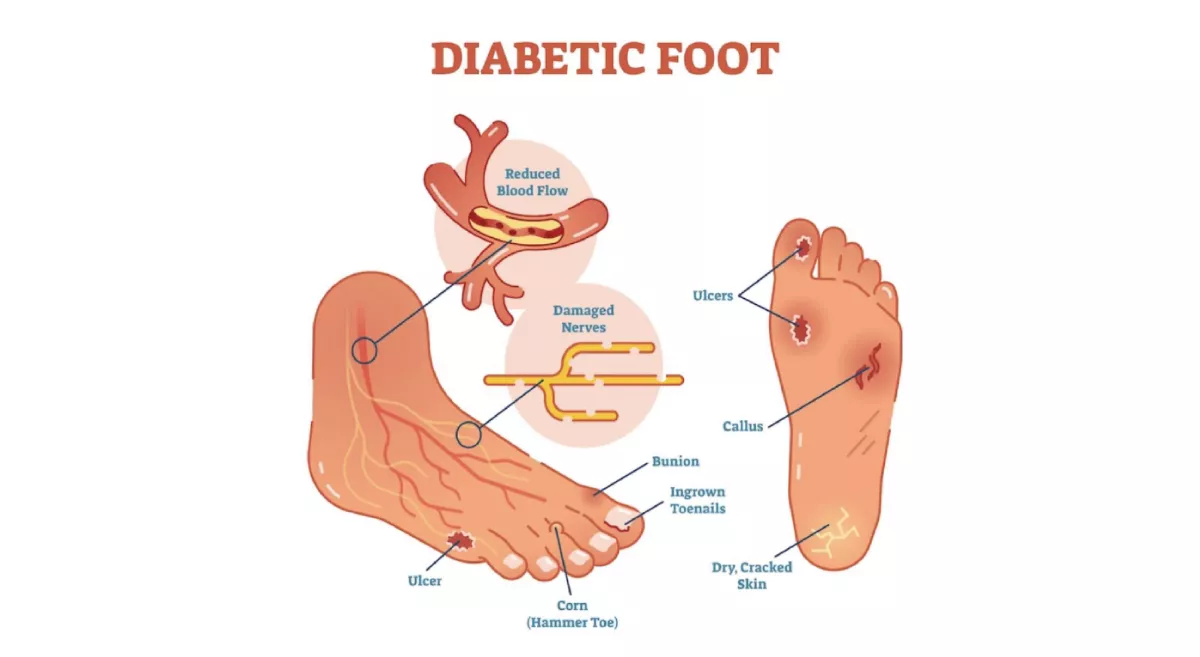
Diabetic foot is a chronic complication of diabetes mellitus that affects the feet and lower extremities. It is a serious condition that can lead to infections, ulcers, and even amputations if left untreated. Managing diabetes and maintaining proper foot care are essential to prevent and manage diabetic foot complications.
What are the causes of diabetic foot?
Diabetic foot can result from several factors, including:
Peripheral neuropathy:
High blood sugar levels can damage the nerves in the feet, leading to reduced sensation. This loss of feeling makes it difficult for individuals to detect injuries or ulcers, which can worsen over time.
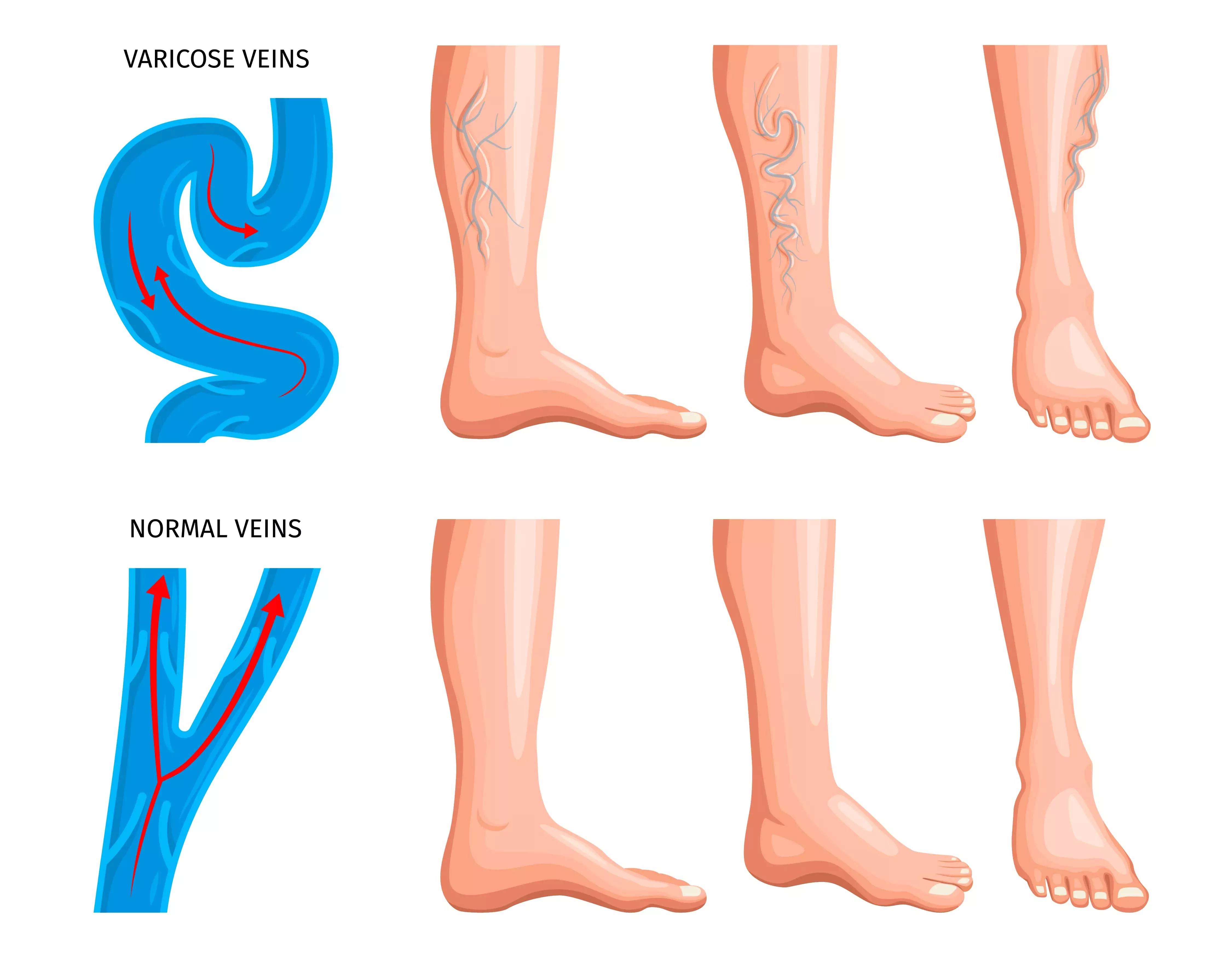
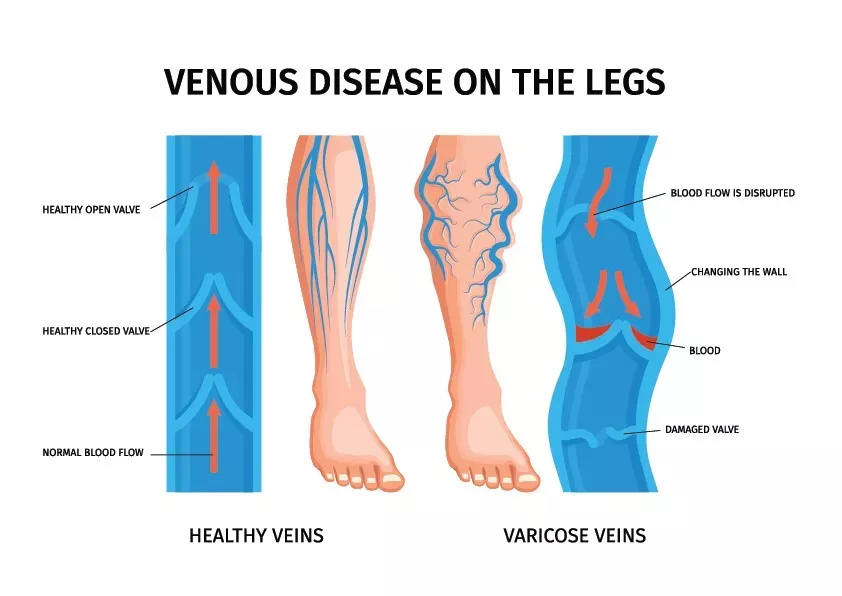
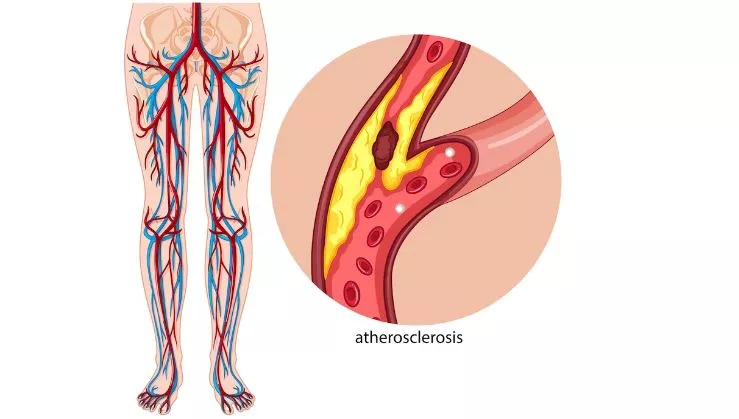
Peripheral arterial disease:
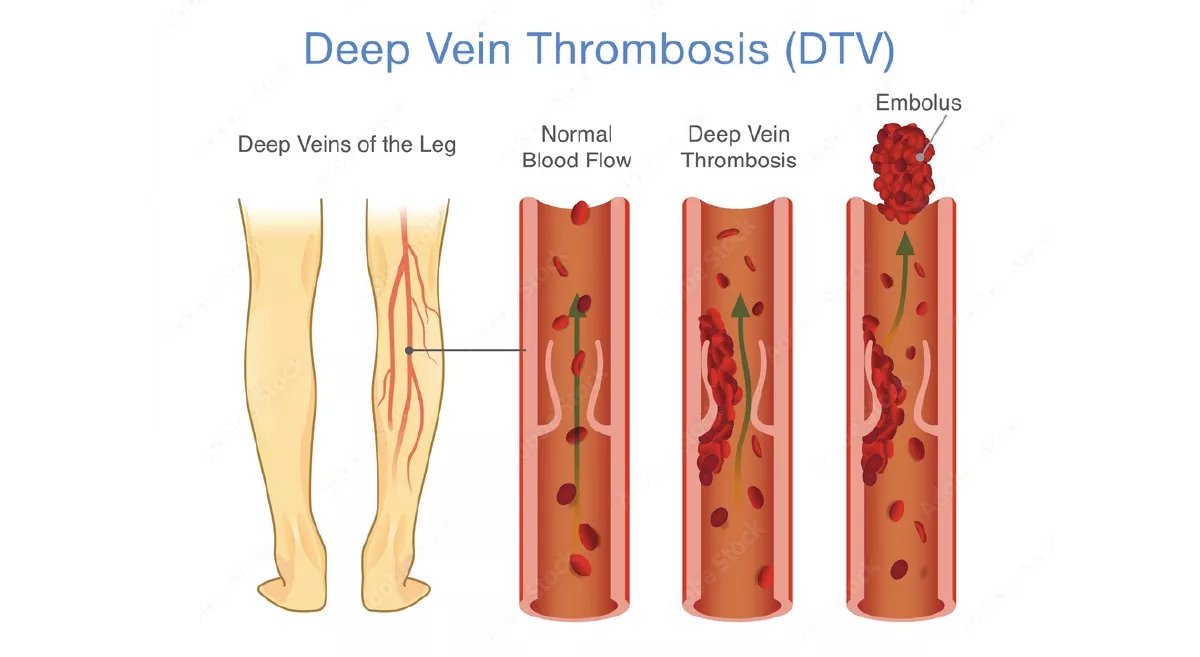
Diabetes can cause narrowing and hardening of the arteries, reducing blood flow to the feet. Inadequate blood supply impairs wound healing and makes the feet more susceptible to infections.
Foot deformities:
Conditions like Charcot foot, hammertoes, and bunions can occur due to nerve and blood vessel damage in diabetes. These deformities can cause abnormal pressure points, leading to ulcers and foot complications.
What are the symptoms of diabetic foot?
The following symptoms may indicate the presence of diabetic foot:
- Numbness or reduced sensation in the feet.
- Tingling or burning sensation.
- Changes in skin colour or temperature.
- Swelling, redness, or inflammation.
- Open sores, ulcers, or wounds that are slow to heal.
- Ingrown toenails or fungal infections.
- Corns or calluses.
- Foot deformities, such as Charcot foot.
How do prevent diabetic foot?
Taking proactive steps to prevent diabetic foot complications is crucial. Here are some preventive measures individuals with diabetes should follow:
Control blood sugar levels:
Maintain good glycaemic control through a healthy diet, regular exercise, and adherence to prescribed medications.
Inspect feet regularly:
Examine the feet daily for any cuts, blisters, sores, or changes in skin colour. Seek medical attention promptly for any abnormalities.
Practice proper foot care:
Wash feet daily with warm water, dry them thoroughly (especially between the toes), and moisturize with a diabetic-friendly lotion. Avoid soaking the feet, as it can dry the skin excessively.
Trim nails carefully:
Cut toenails straight across and avoid cutting too close to the skin to prevent ingrown toenails.
Wear appropriate footwear:
Choose well-fitting shoes with enough room for the toes, and opt for breathable materials. Avoid open-toed shoes and high heels that can cause pressure points.
Protect feet from extreme temperatures:
Use warm socks and insulated shoes during cold weather and avoid exposing feet to excessive heat.
How do we treat Diabetic foot?
Treatment for diabetic foot depends on the severity of the condition and may include:
- Wound care: Proper cleaning and dressing of foot ulcers or wounds to promote healing and prevent infection.
- Offloading pressure: The use of specialized shoes, braces, or casts to redistribute pressure and relieve pressure points.
- Infection management: Antibiotics may be prescribed to treat infections, and in severe cases, surgical intervention may be required to drain abscesses or remove infected tissue.
- Vascular intervention: In cases of impaired blood flow, interventions like angioplasty or bypass surgery may be necessary to restore adequate circulation.
- Diabetic foot education: Patients should receive education on foot care techniques, self-examination, and when to seek medical help.