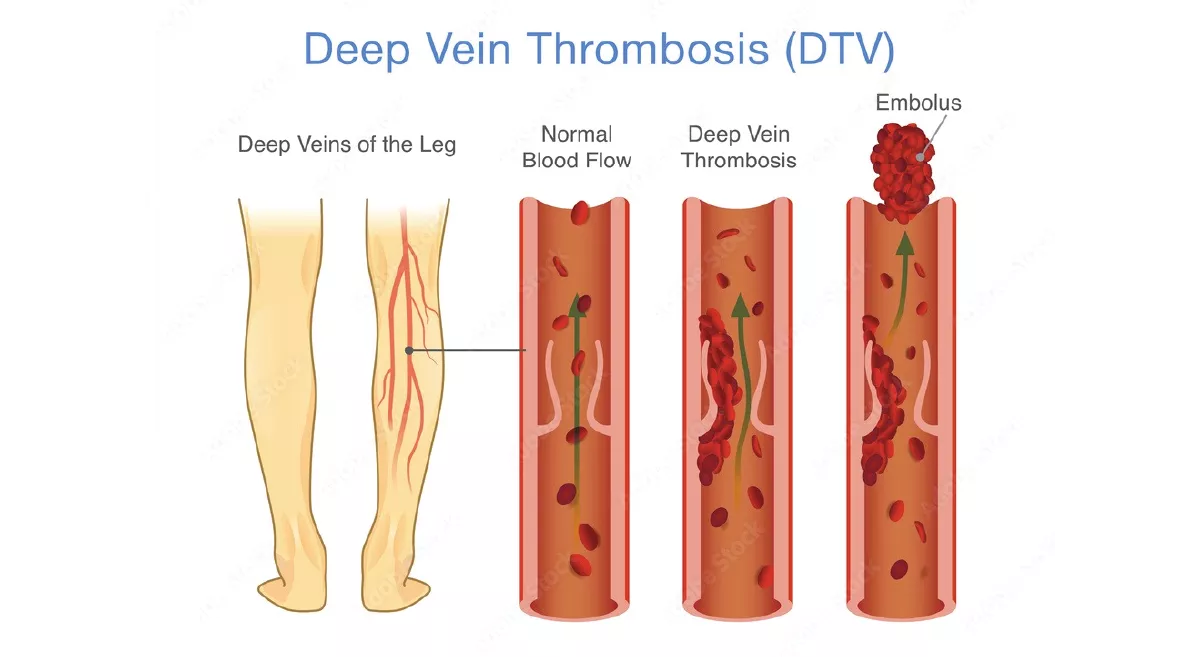
Deep vein thrombosis (DVT) is formation of blood clot in deep veins, most commonly in the legs or pelvis. A minority of DVTs occur in the arms.. It is important to know about DVT because it can happen to anyone and can cause serious illness, disability, and in some cases, death. The good news is that DVT is preventable and treatable if discovered early.
What are the symptoms of DVT?
Swelling in the affected leg or rarely swelling in both the legs. Cramping pain or soreness which starts in the calf, leading to pain in the entire leg. Redness or discoloured skin on the leg. Warm feeling in the affected leg. DVT sometimes occurs without noticeable symptoms.
What are the complications of DVT?
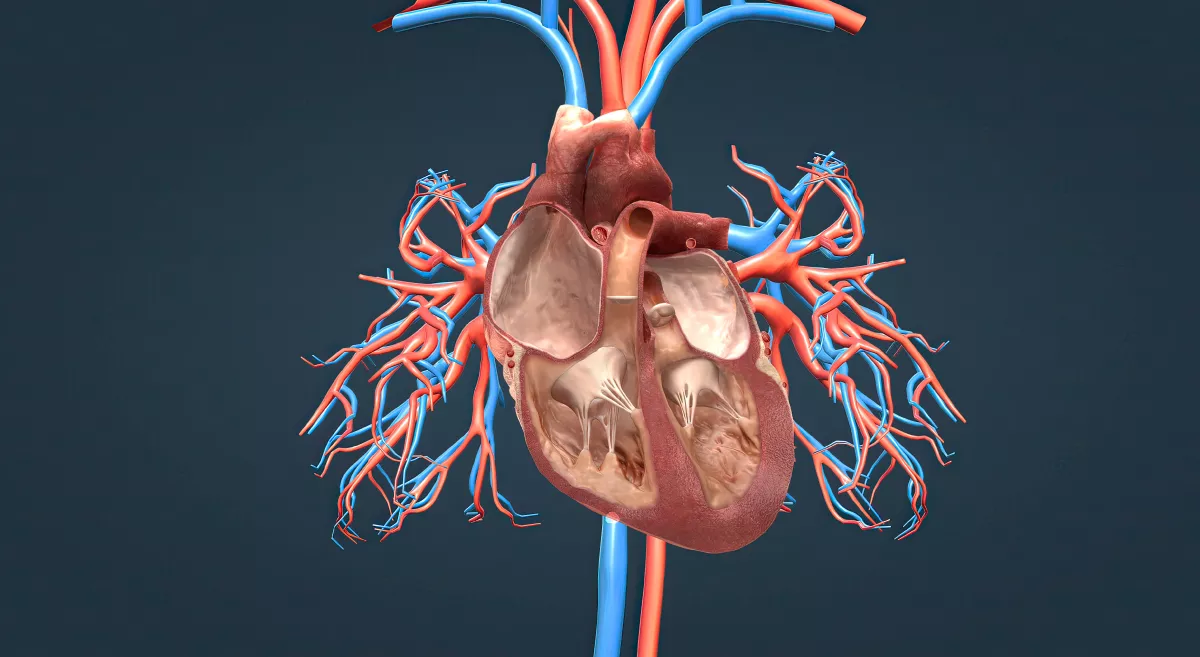
The most serious complication of DVT happens when a part of the clot breaks off and travels through the bloodstream to the lungs, causing a blockage called pulmonary embolism (PE). If the clot is small, and with appropriate treatment, people can recover from PE. However, if the clot is large, it can stop blood from reaching the lungs and is fatal.
One-third of people who have DVT will have long-term complications caused by the damage the clot does to the valves in the veins called post-thrombotic syndrome (PTS). People with PTS have symptoms such as swelling, pain, discoloration, and in severe cases, scaling or ulcers in the affected part of the body. In some cases, the symptoms can be severely disabling to the patient.
DVT and PE can become a chronic illness; about 30% of people who have had DVT or PE are at risk for another episode.
What are the risk factors for developing DVT?
Anyone can develop DVT. However, certain factors can increase the chances of having this condition. The risk increases even more for someone who has more than one of these risk factors at the same time. Some of them are:
- Injury to vein, like in: fractures, severe muscle injury, or major surgery.
- Slow blood flow, such as: confinement to bed (due to a medical condition), limited movement (cast on a leg to help heal an injured bone), sitting for a long time (long duration of travel) or paralysis.
- Increased estrogen, such as: birth control pills, hormone replacement therapy and pregnancy.
- Certain chronic medical illnesses, such as: heart disease, lung disease, cancer and its treatment and inflammatory bowel disease.
- Other factors that increase the risk of DVT include: Previous DVT or PE, family history of DVT or PE, age (risk increases as age increases), obesity and Inherited clotting disorders.
How to diagnose DVT?
The diagnosis of DVT or PE requires special tests that can only be performed by a doctor. Which is why it is important for you to seek medical care if you experience any of the symptoms of DVT or PE. The doctors might suggest following tests which include –
- Ultrasound: An ultrasound helps to determine where the clot is, whether it is growing or to check for a new one.
- Blood Test: Some basic blood tests are done to determine what form of treatment would be suitable. Advanced tests are also carried out, when needed, to determine if there are any underlying blood problems that make you more prone to developing clots. Some of these tests are carried out immediately and some a while later.
- CT or MRI scans: These can help in providing visual images of the veins and showing the clot, if it exists. Sometimes the clots are revealed when scanning for other reasons.
- Venography: A dye is injected into a large vein in the foot or ankle. An X-ray creates an image of the veins in the legs and feet, to look for clots. However, less invasive methods of diagnosis, such as ultrasound, can usually confirm the diagnosis. This is therefore used only as a part of a treatment strategy.
What are the treatment strategies available to treat DVT?
If a person develops symptoms of DVT, they may have to be started with injection of an anticoagulant (blood thinning) medicine called heparin while they are waiting for an ultrasound scan to tell if they have DVT.
After DVT is diagnosed, the main treatment is tablets of an anticoagulant medicine, such as warfarin or other newer oral anticoagulants such as rivaroxaban. Which has to be probably taken for at least 3 months.
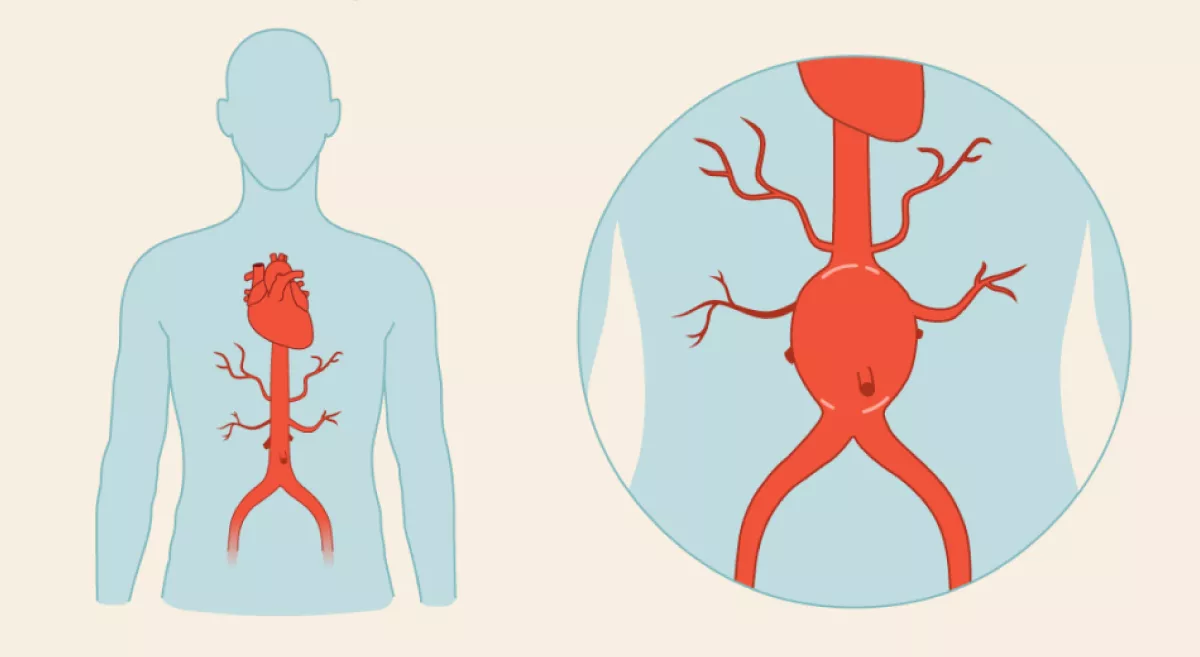
If anticoagulant medicines are not suitable, they may have to place a filter into a large vein – the inferior vena cava – in their abdomen. The filter traps and stops the blood clot from travelling to the heart and lungs thereby preventing Pulmonary Embolism.
A newer treatment involves breaking up and sucking out the clot through a small tube in the vein (Catheter directed thrombolysis or Mechanochemical aspiration of thrombus) thereby preventing post thrombotic syndrome.
DVT in pregnancy is treated differently with anticoagulant injections for the rest of the pregnancy and until the baby is 6 weeks old.
How to prevent DVT?
- The risk of having DVT can be lowered by making lifestyle changes like maintaining optimal blood pressure, quit smoking and losing weight if overweight.
- Being mobile and walking around after sitting for too long helps to keep the blood flowing.
- Keep moving around often, get out of the car and stretch at intervals during long drives.
- Walk along the aisles if flying, taking a train, or riding a bus. Stretch your legs and move your feet while sitting — this keeps the blood moving steadily in the calves.
- Don’t wear tight clothes that can restrict blood flow while traveling for long durations.
- Make sure you do not get dehydrated, drink plenty of water especially in hot weather and when travelling or having a fever.
- Take blood thinners on doctor’s recommendation to lower the chances of blood clot post a surgery (if having one).