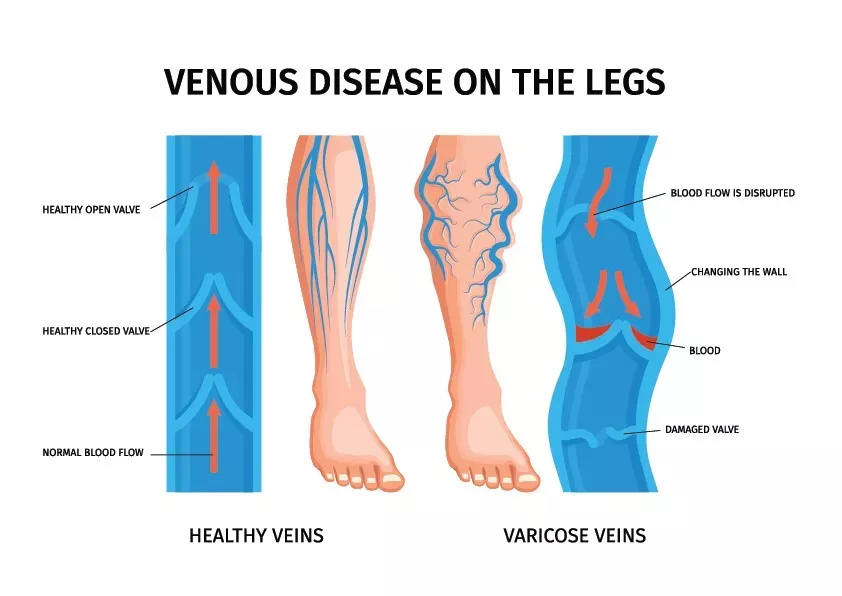
Peripheral vascular disease, also known as peripheral artery disease (PAD), is a condition that affects the blood vessels outside of the heart and brain. It primarily involves the narrowing or blockage of arteries that supply blood to the legs, arms, stomach, or kidneys.
What causes peripheral vascular disease?
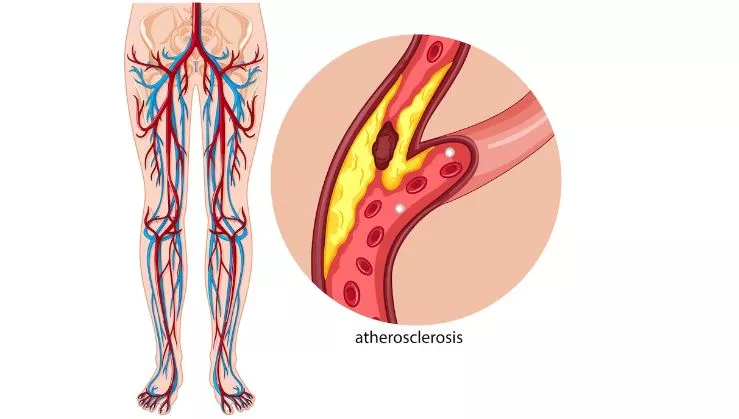
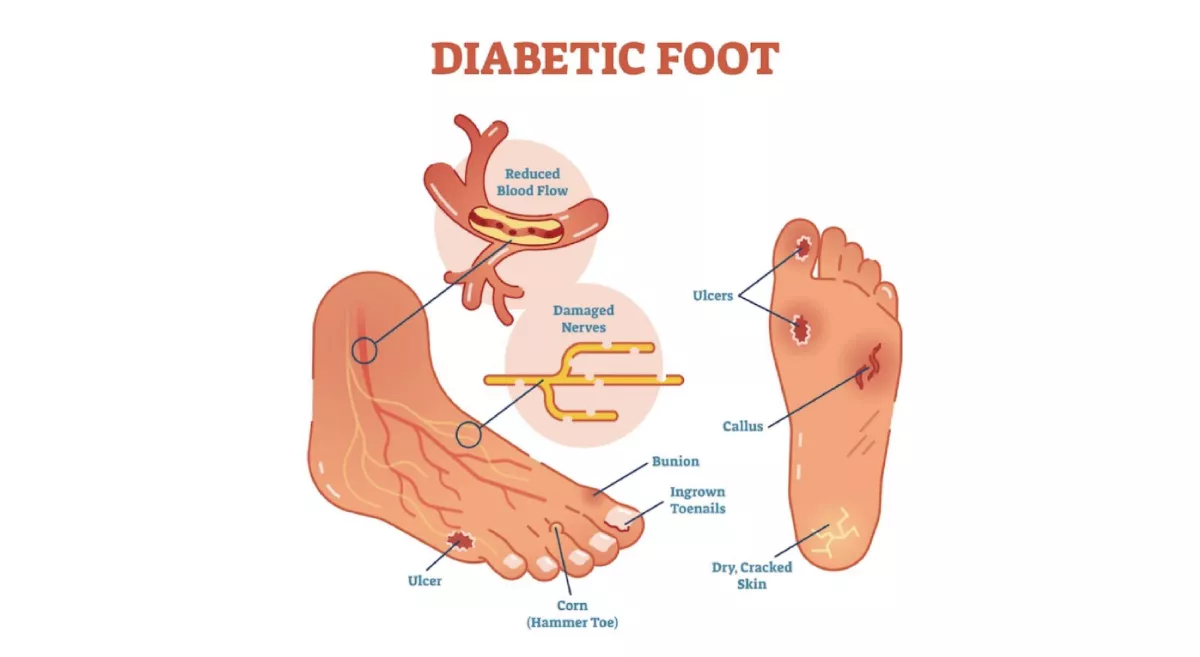
The most common cause of peripheral vascular disease is atherosclerosis, which is the build-up of fatty deposits (plaque) inside the arteries. Other factors that contribute to PVD include smoking, diabetes, high blood pressure, high cholesterol, obesity, and a family history of the disease.
What are the symptoms of peripheral vascular disease?
Some individuals with peripheral vascular disease may not experience any symptoms. However, common symptoms include pain, cramping, or fatigue in the muscles of the legs or arms during activity (intermittent claudication). Other symptoms may include numbness, tingling, weakness, coldness, or colour changes in the affected area, slow-healing wounds, and erectile dysfunction in men.
How is peripheral vascular disease diagnosed?
A diagnosis of peripheral vascular disease is typically made through a combination of medical history evaluation, physical examination, and diagnostic tests. These tests may include ankle-brachial index (ABI) measurement, which compares the blood pressure in the arms and legs, Doppler ultrasound, angiography, or magnetic resonance angiography (MRA).
Can peripheral vascular disease be treated?
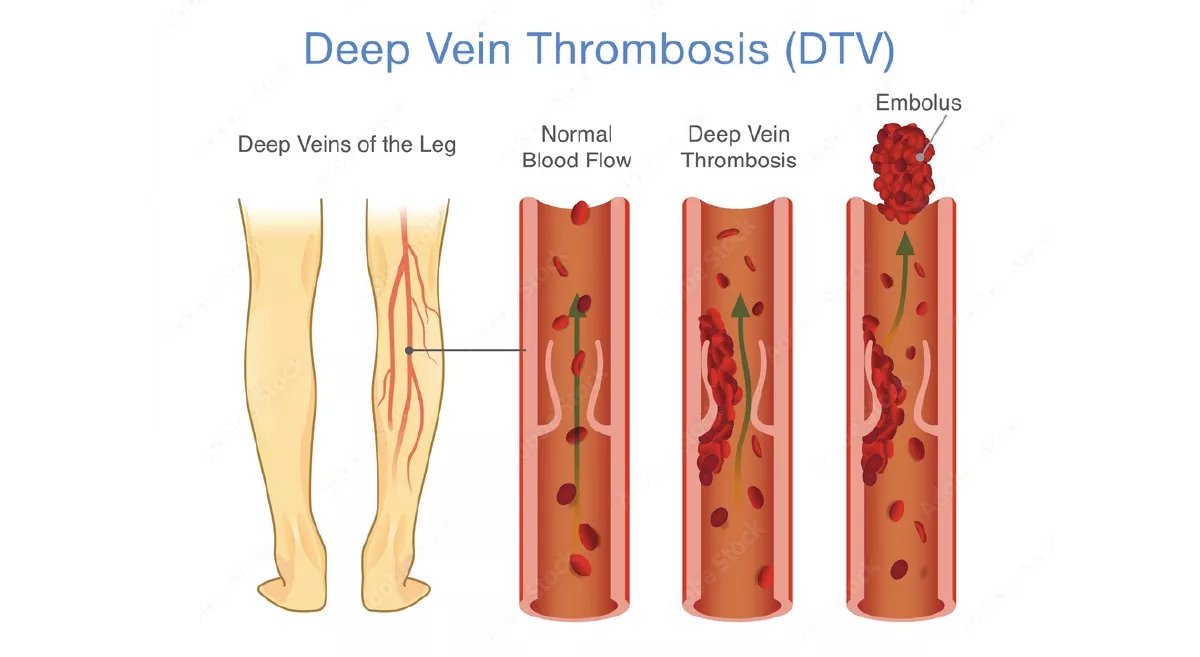
Yes, there are several treatment options available for peripheral vascular disease. Lifestyle modifications such as quitting smoking, adopting a healthy diet, exercising regularly, and managing conditions like diabetes, high blood pressure, and high cholesterol are crucial. Medications may be prescribed to control symptoms, improve blood flow, and prevent blood clots. In some cases, procedures such as angioplasty, stenting, or bypass surgery may be necessary to restore blood flow.
Can peripheral vascular disease be prevented?
While it may not always be possible to prevent peripheral vascular disease entirely, certain lifestyle choices can significantly reduce the risk. Quitting smoking, maintaining a healthy weight, engaging in regular physical activity, managing chronic conditions, and following a balanced diet can all help prevent or delay the onset of PVD.
What are the complications of peripheral vascular disease?
If left untreated, peripheral vascular disease can lead to various complications. Severe blockages may result in tissue damage, non-healing wounds, and ulcers, which can potentially lead to infections or gangrene. In extreme cases, critical limb ischemia may occur, which is characterized by severe pain, ulcers, and tissue death. Peripheral vascular disease is also associated with an increased risk of heart attack, stroke, and other cardiovascular events.
Is peripheral vascular disease a serious condition?
Yes, peripheral vascular disease is a serious condition that requires medical attention. It not only causes discomfort and reduces mobility but also increases the risk of complications such as limb loss, heart disease, and stroke. However, with appropriate management and lifestyle changes, the progression of the disease can be slowed down, and symptoms can be alleviated. Early diagnosis and treatment are crucial for better outcomes.
Can peripheral vascular disease affect other parts of the body besides the legs and arms?
Yes, while peripheral vascular disease commonly affects the blood vessels in the legs and arms, it can also impact other areas of the body. In some cases, the arteries supplying blood to the stomach, intestines, or kidneys can be affected, leading to conditions like mesenteric ischemia or renal artery disease. These conditions can cause abdominal pain, digestive issues, and kidney problems.
Are there any self-care measures that can help with peripheral vascular disease?
Yes, there are self-care measures that can help manage peripheral vascular disease. These include quitting smoking, following a healthy diet low in saturated and trans fats, engaging in regular exercise, maintaining a healthy weight, controlling blood sugar levels (if diabetic), managing blood pressure and cholesterol levels, and properly caring for wounds or ulcers to prevent infections. It is important to consult with a vascular surgeon for personalized advice and guidance on self-care measures.