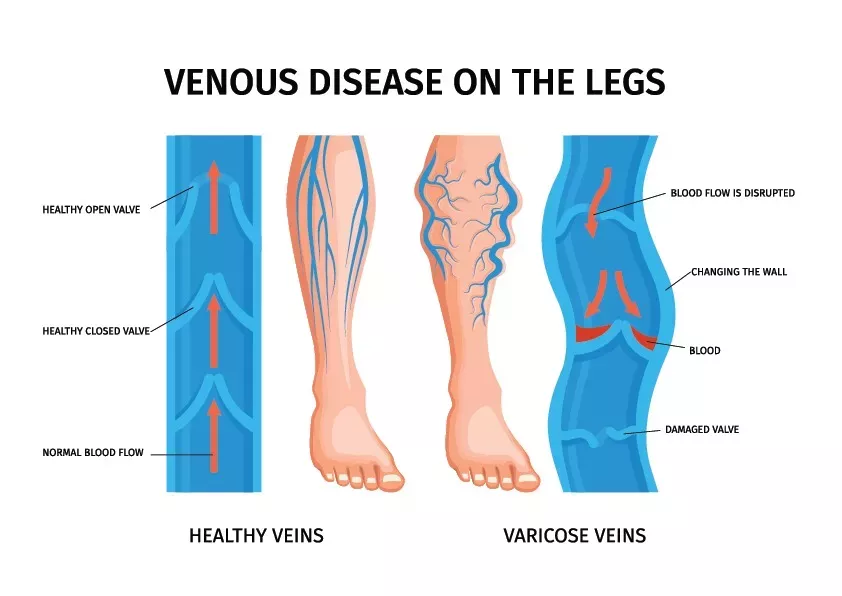
Varicose veins are a common condition that affects the veins, usually in the legs, causing them to become enlarged, twisted, and bulging. They occur when the valves within the veins fail to function properly, leading to blood pooling and increased pressure within the affected veins.
While varicose veins are often considered a cosmetic concern, they can also cause discomfort, pain, and other complications. Fortunately, various treatment options are available to manage and treat varicose veins effectively.
What are the causes of Varicose Veins?
Age and Genetics:
As we age, the natural wear and tear on vein valves can lead to their dysfunction. Additionally, a family history of varicose veins increases the likelihood of developing this condition.
Prolonged Standing or Sitting:
Occupations that require long periods of standing or sitting can put additional pressure on the veins, hindering blood flow and increasing the risk of varicose veins.
Hormonal Changes:
Hormonal fluctuations during pregnancy and menopause can weaken vein walls and valves, making women more susceptible to varicose veins.
Obesity:
Excess weight puts added pressure on the veins, impairing their ability to transport blood efficiently and potentially leading to the development of varicose veins.
When is procedure for Varicose Vein required?
Treatment for varicose veins is typically recommended when the symptoms and complications associated with them become bothersome or when they significantly impact an individual's quality of life. Some common indications for varicose vein procedures include:
Pain and Discomfort:
When varicose veins cause persistent pain, throbbing, aching, or cramping in the legs, treatment may be advised to alleviate these symptoms.
Swelling and Inflammation:
Varicose veins can lead to swelling, inflammation, and a feeling of heaviness in the affected leg. Treatment may be considered to reduce these symptoms.
Skin Changes:
Skin discoloration, rashes, dryness, and itchiness around the varicose veins can indicate the need for treatment to prevent further skin complications.
Ulcers and Bleeding:
In rare cases, varicose veins can develop ulcers or skin sores, which are often difficult to heal. Additionally, if the veins are prone to bleeding, medical intervention may be required.
What are the available treatment options for Varicose Veins:
Several treatment options are available for varicose veins, depending on the severity and specific needs of the patient. These procedures aim to relieve symptoms, improve appearance, and prevent complications. Here are some commonly used treatments:
Lifestyle Changes:
Simple lifestyle modifications such as regular exercise, maintaining a healthy weight, avoiding prolonged periods of standing or sitting, and elevating the legs can alleviate symptoms and prevent further progression.
Compression Stockings:
Wearing compression stockings provides external pressure that helps improve blood circulation and reduces discomfort associated with varicose veins.
Endo-venous Laser Ablation (EVLA):
EVLA is a minimally invasive treatment that uses laser energy to heat and seal off the affected vein. It is effective for larger varicose veins can be performed under local anaesthesia.
Radiofrequency Ablation (RFA):
Similar to EVLA, RFA involves using heat energy to close off the damaged vein. A catheter with a radiofrequency device is inserted into the vein to achieve this.
Ambulatory Phlebectomy:
This surgical procedure involves making tiny incisions over the varicose veins and removing them through these small cuts. Ambulatory phlebectomy is suitable for larger varicose veins close to the surface of the skin.
Sclerotherapy:
This procedure involves injecting a solution directly into the affected vein, causing it to close and eventually fade away. Sclerotherapy is commonly used for smaller varicose veins and spider veins.
High Ligation and Vein Stripping:
This traditional surgical procedure involves tying off the affected vein and removing it through small incisions. It is typically reserved for severe cases or when other treatments have been unsuccessful.
Conclusion:
Varicose veins can be both a cosmetic concern and a potential health issue. Understanding the causes, recognizing the symptoms, and exploring the available treatment options are essential for managing this condition effectively. If you suspect you have varicose veins or are experiencing any related symptoms, it is advisable to consult a vascular surgeon who can provide an accurate diagnosis and recommend the most appropriate course of action.
Remember, maintaining a healthy lifestyle, including regular exercise, maintaining a healthy weight, and avoiding prolonged periods of inactivity, can play a significant role in preventing or managing varicose veins. Taking proactive steps to care for your vascular health can go a long way in ensuring your overall well-being and quality of life.