Peripheral Vascular Disease (PVD) is a common complication for those with diabetes, significantly impacting blood flow and increasing the risk of severe complications like infections, ulcers, and in some cases, amputation. This blog will explore the connection between diabetes and PVD, shedding light on risk factors, early symptoms, and treatment options to help manage and reduce the impact of this condition.
What is Peripheral Vascular Disease?
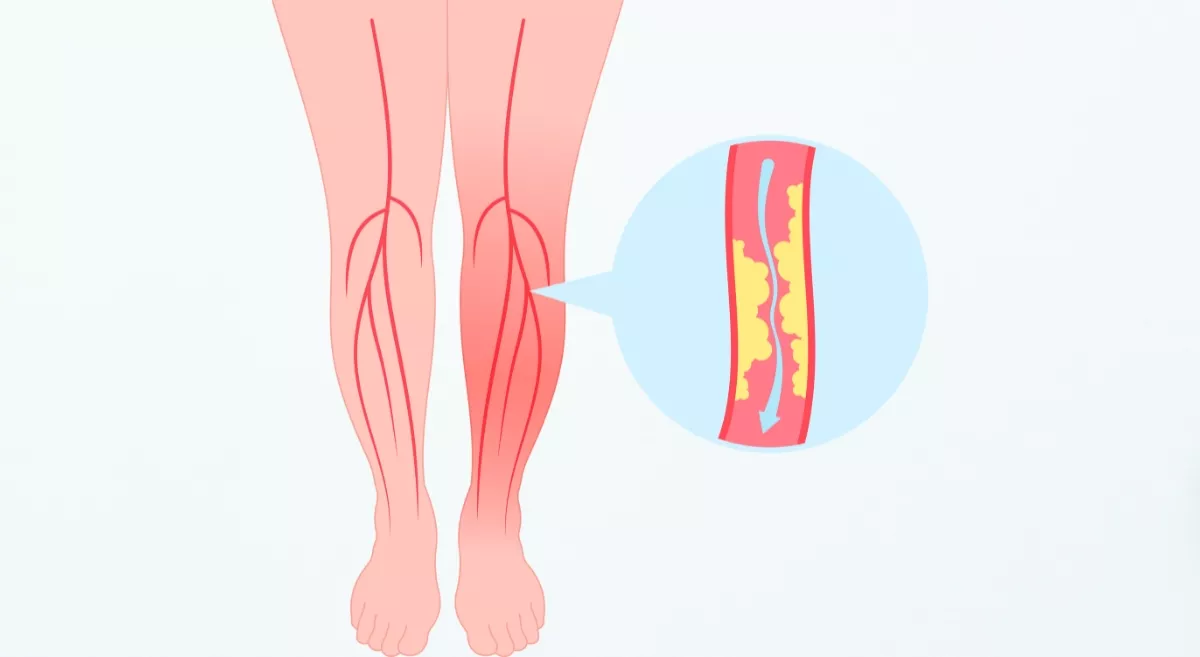
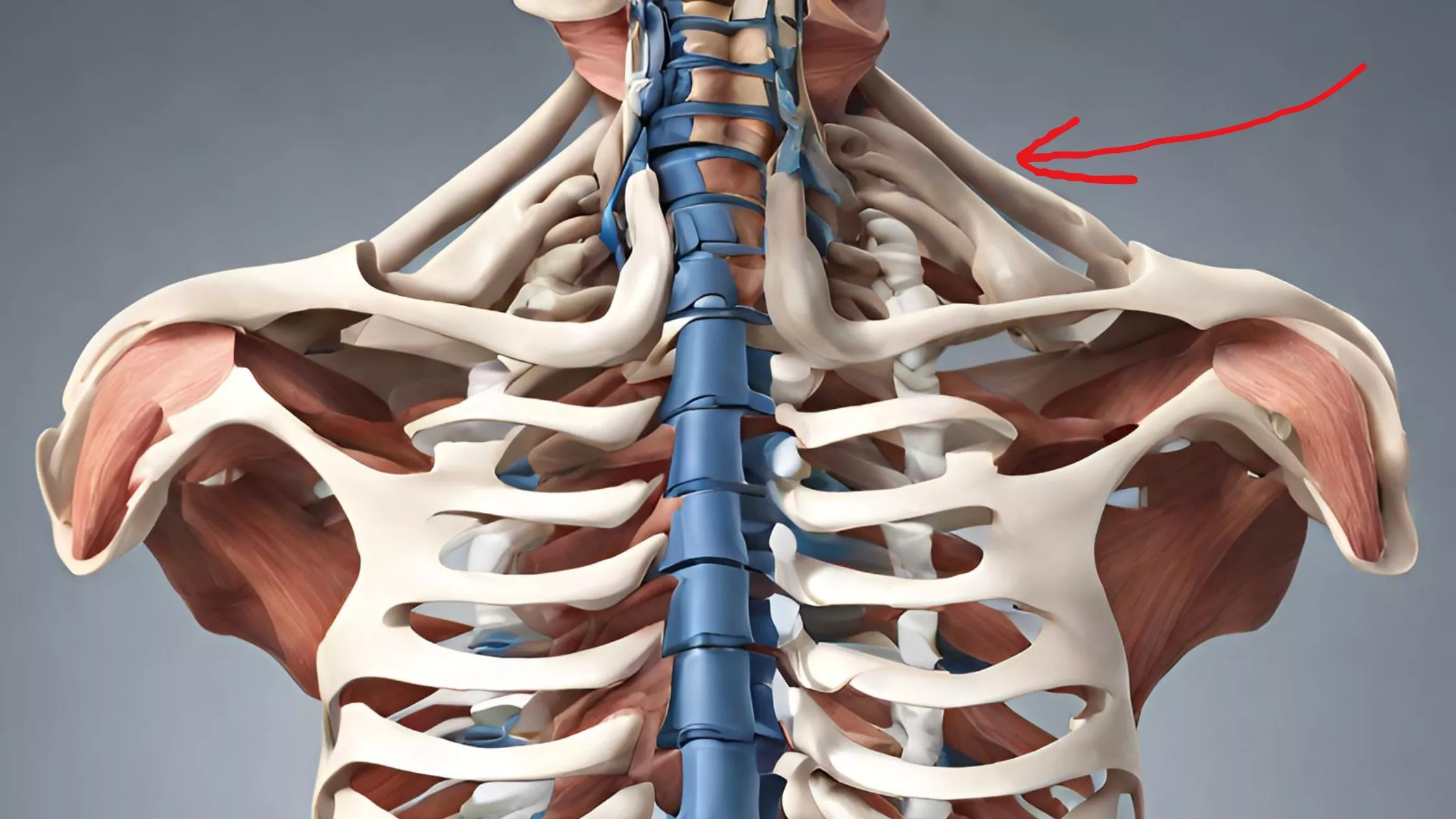
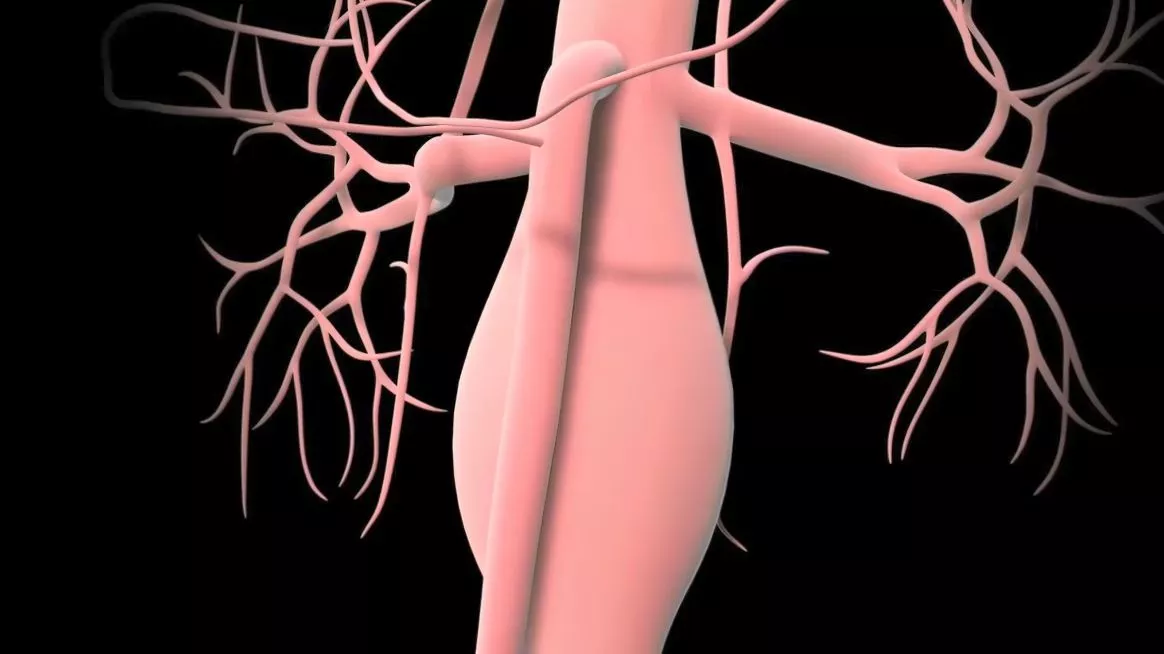
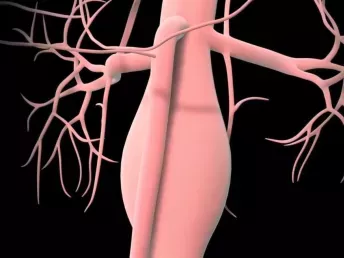
Peripheral Vascular Disease, commonly called peripheral artery disease (PAD), is a form of circulatory problem that leads to the constriction of blood vessels, causing decreased blood supply to the limbs, particularly the legs. This happens due to atherosclerosis, where a formation called plaque is deposited on the inner walls of the arteries, hence narrowing them and increasing the chances of blood clot formation. Because blood supply is critical in the healing process of the skin and other layers of the body tissues, the lack of blood circulation may result in some uncomfortable signs and additional damaging consequences.
Why Diabetics are Prone to PVD
Diabetes is an illness that impacts blood glucose but is also associated with changes in blood vessels and circulation throughout the body. Diabetes causes high blood glucose, which leads to damage within vessel walls to form plaques and narrowing of the arteries. Also, in diabetics, the duration of blood vessel inflammation is likely to be higher than in patients without diabetes, which increases the risk of PVD.
Individuals with diabetes face an increased likelihood of developing PVD for several key reasons:
- Chronic Hyperglycemia: High blood sugar also negatively impacts the blood vessels by damaging the cells lining the blood vessels and hence promotes the accumulation of fatty deposits.
- Diabetic Neuropathy: Nerve damage can result in a loss of sensation, particularly in the feet, which may mask symptoms of PVD.
- Increased Inflammation and Oxidative Stress: Patients with diabetes usually have higher levels of inflammation, which increases the hardness of arteries.
What are Common Risk Factors for PVD in Diabetics?
Though diabetes itself is a significant risk factor, other elements can contribute to the development and progression of PVD:
- Smoking: Smoking is found to contribute to worsening atherosclerosis and also damages blood vessels, hence posing serious risks for diabetics.
- Hypertension (High Blood Pressure): High blood pressure raises the stress on the arterial walls, which in turn worsens blood vessel deterioration.
- Dyslipidemia: Plaque builds up if the patient has high levels of bad cholesterol (LDL) and low levels of good cholesterol (HDL).
- Age and Gender: People who are 50 and above, and men are more susceptible to developing PVD than women.
Symptoms that Indicate PVD in Diabetics:
Some of the PVD symptoms are not prominently noticeable or are even different from the common features traditionally associated with the disease, which worsens this situation for diabetics. Common symptoms include:
- Claudication: Pain, cramping, or heaviness in the legs or buttocks that occurs during walking and is relieved by rest.
- Coldness in the Extremities: One may feel cold due to reduced blood flow to the feet or legs.
- Poor Healing of Sores and Ulcers: There is poor circulation in the feet, thus it takes longer for injuries to heal fully.
- Shiny Skin or Loss of Hair on the Legs and Feet: When circulation is reduced, it changes skin texture and also the rate of hair growth.
- Reduced Pulse in the Legs and Feet: Lack of or weak pulse in the legs indicates limited blood circulation.
Complications of PVD in Diabetics
Untreated or unmanaged PVD can lead to severe complications. Due to compromised blood flow, even minor injuries can develop into chronic ulcers, and infections may spread more quickly. Some potential complications include:
- Non-Healing Wounds and Ulcers: These may progress to infection and, without adequate blood flow, be challenging to treat.
- Increased Risk of Infection: Reduced circulation leads to an environment where bacteria can flourish.
- Amputation: When tissue damage becomes extensive and unmanageable, amputation may be necessary to prevent further health risks.
- Critical Limb Ischemia (CLI): This severe form of PVD results in constant pain, skin ulcers, and even gangrene.
How to Know if I Have PVD?
Studies demonstrate that recognizing PVD in diabetic persons is important, especially in the initial stages of the disease. Various tests are available to confirm a PVD diagnosis:
- Ankle-Brachial Index (ABI): This is a non-invasive test, whereby blood pressure in the ankle is compared with blood pressure in the arm. A low ABI value shows less blood circulation.
- Doppler Ultrasound: An ultrasound scan will reveal the constriction of arteries as well as any occlusions.
- Magnetic Resonance Angiography (MRA): Though this test gives clear images of blood vessels, it also shows locations with reduced blood flow.
- Angiogram: This technique utilizes a contrast dye wherein obstructions in the arteries are illuminated through X-ray visuals.
How to Treat Peripheral Vascular Disease in Diabetic Patients?
Managing PVD in diabetic patients typically requires a combination of lifestyle changes, medications, and in some cases, surgical intervention. The primary goal of managing SLE is the relief of symptoms, promotion of circulation, and avoiding further advancement of the illness.
- Lifestyle Modifications
- Smoking Cessation: You need to quit smoking to stop the progression of PVD. Smoking acts as a barrier to blood flow and also affects blood vessels.
- Exercise Therapy: In more chronic cases, supervised exercise programs such as walking are suggested as they improve circulation, hence alleviating patients’ symptoms.
- Dietary Changes: Low fat, high fiber, fruits, and vegetable diets lower cholesterol and balance blood glucose concentrations.
- Medications
Several medications may be prescribed to help manage PVD in diabetics:- Antiplatelet Agents: Drugs such as aspirin or clopidogrel thin the blood so that it flows more easily through the arteries and limits clot formation.
- Cholesterol-Lowering Medications: Statins for cardiac care reduce cholesterol values in the blood and lower the rate of atherosclerotic plaque formation.
- Blood Pressure Medications: Controlling blood pressure reduces arterial stress and helps prevent PVD progression.
- Blood Sugar Control: Ensuring the patient’s blood sugar is well-controlled is another way to avoid worsening of blood vessels.
- Surgical and Interventional Procedures
In cases of advanced PVD, lifestyle changes and medication might not be enough; surgical options may be necessary:- Angioplasty and Stenting: A minimally invasive procedure in which the artery is expanded by the inflation of a balloon, with a stent put in the artery to maintain its open state.
- Atherectomy: A process where plaque is removed to open the arteries and allow regular blood flow.
- Bypass Surgery: In more severe cases, bypass surgery can be an option, creating an alternate pathway for blood flow around narrowed or blocked arteries.
Can Peripheral Vascular Disease be Prevented?
The best way to avoid PVD in diabetics begins with blood glucose control along with periodic screening by the primary care physician. Additional preventive steps include:
- Routine Foot Examinations: Diabetics should check their feet every day for cuts, blisters, or sores that can easily develop into infections.
- Regular Medical Screenings: Doppler ultrasounds and ABI tests can reveal early signs of PVD, ensuring timely handling by patients and clinicians.
- Maintain Optimal Blood Pressure and Cholesterol Levels: Keeping these levels within a healthy range minimizes the risk of vascular complications.
Conclusion
Peripheral Vascular Disease is a potentially dangerous complication of diabetes that can result in profound consequences for affected patients. Although there are no known cures for PVD, diabetics can prevent its progression by taking the preventive and treatment measures outlined here. Proper management of diabetes through periodic check-ups, lifestyle changes, and necessary medications helps those with diabetes experience a less severe condition of PVD and retain improved mobility and quality of life.