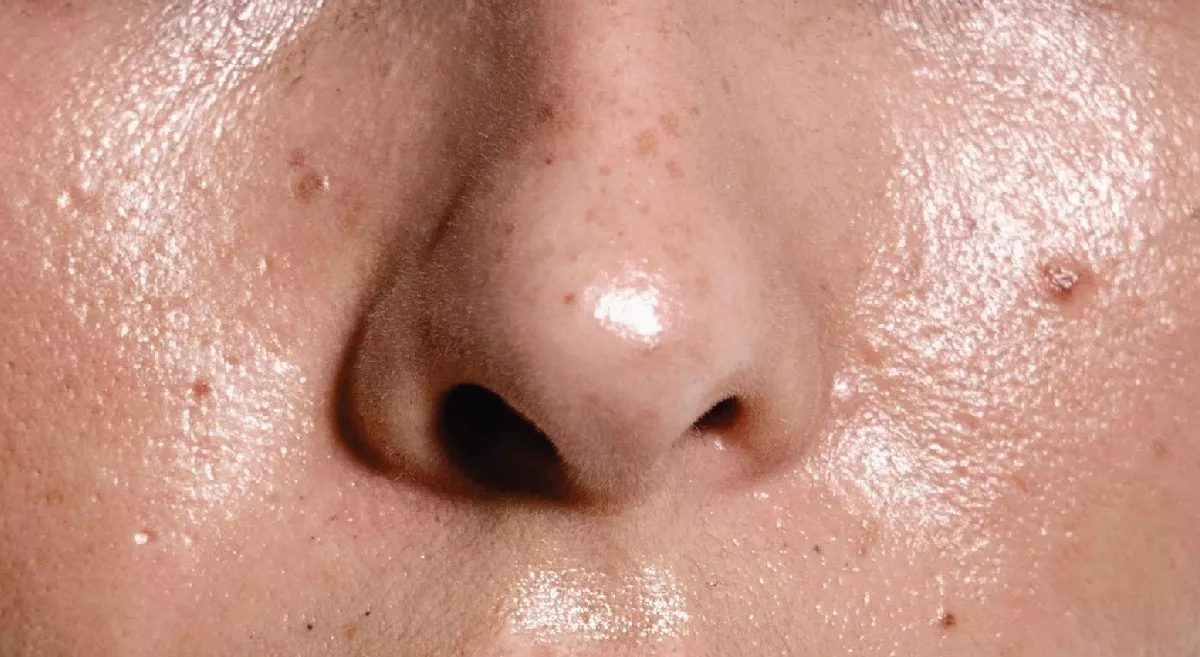
Psoriasis is a chronic autoimmune condition that primarily affects the skin, causing red, scaly patches. Here’s an overview of its causes :
Causes
- Genetics: Family history can increase the likelihood of developing psoriasis.
- Immune System: An overactive immune response leads to rapid skin cell growth and inflammation.
- Environmental Triggers: Factors such as stress, infections, skin injuries, certain medications, and weather changes can trigger or exacerbate psoriasis.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and obesity can also contribute to the severity of the condition.
CURABILITY
Psoriasis is a chronic autoimmune condition that currently has no cure. However, there are various treatment options that can help manage symptoms and reduce flare-ups.
While psoriasis can be managed effectively, ongoing treatment may be necessary to keep symptoms under control. Regular consultations with a healthcare provider are essential to tailor treatment plans based on individual needs
SPREADABILITY
Psoriasis is not contagious; it cannot be spread from person to person through skin contact, sharing personal items, or any other means. Instead, it is an autoimmune condition that involves an overactive immune response leading to inflammation and rapid skin cell production.
While the exact cause of psoriasis is not fully understood, it is believed to be influenced by a combination of genetic, environmental, and immune factors. Some common triggers for flare-ups include:
- Stress
- Infections (like strep throat)
- Skin injuries (cuts, scrapes, sunburn)
- Weather (cold, dry conditions)
- Certain medications (like beta-blockers or lithium)
- Heavy alcohol consumption or smoking
Understanding and avoiding personal triggers can help manage the condition and reduce the frequency and severity of flare-ups.
INFECTIOUSNESS OF PSORIASIS
Psoriasis is not infectious; it cannot be transmitted from one person to another. It is an autoimmune condition, meaning it arises from a malfunction in the immune system rather than an infectious agent like a virus or bacteria.
While psoriasis can sometimes be triggered by infections or environmental factors, the condition itself is solely related to genetic and immune system responses. People with psoriasis often face social misconceptions about the disease due to its visible symptoms, but it’s important to emphasize that there’s no risk of spreading it to others.
AWARENESS AND TREATMENT
Awareness and treatment of psoriasis are essential for managing the condition effectively. Here are some key points regarding both:
Awareness
- Understanding the Condition: Psoriasis is a chronic autoimmune disorder that primarily affects the skin but can also have systemic implications. Awareness helps in recognizing symptoms like red patches of skin covered with thick, silvery scales.
- Common Misconceptions: Many people mistakenly believe psoriasis is contagious. Education is crucial to dispel these myths and reduce stigma.
- Impact on Quality of Life: Psoriasis can significantly affect mental health and quality of life. Awareness of the emotional and psychological aspects is important for support and treatment.
- Triggers: Being aware of common triggers (stress, infections, skin injuries) can help individuals manage their condition and prevent flare-ups.
TREATMENT OPTIONS
1.Topical Treatments:
- Corticosteroids: Reduce inflammation and slow skin cell turnover.
- Vitamin D Analogues: Help to slow skin cell growth.
- Topical Retinoids: Promote skin cell turnover and reduce inflammation.
- Coal Tar: Can reduce scaling, itching, and inflammation
2.Phototherapy:
- UVB Therapy: Exposure to ultraviolet B light helps slow skin cell turnover.
- PUVA: A combination of a drug (psoralen) and UVA light.
3.Systemic Medications (for moderate to severe psoriasis):
- Oral Medications: Such as methotrexate, cyclosporine, and acitretin.
- Biologics: Target specific parts of the immune system (e.g., TNF-alpha inhibitors, IL-17 inhibitors).
4.Lifestyle and Home Remedies:
- Moisturizers: Keeping skin hydrated can help manage dryness and scaling.
- Stress Management: Techniques like yoga, meditation, and exercise may help reduce flare-ups.
- Diet: Some people find that anti-inflammatory diets or specific food changes improve their symptoms.
5. Regular Follow-ups:
- Ongoing communication with healthcare providers is essential for adjusting treatment plans as needed and monitoring the condition.
CONCULSION
Increasing awareness and understanding of psoriasis among patients, healthcare providers, and the general public can lead to better management and support for those affected. If you or someone you know has psoriasis, it's beneficial to consult with a dermatologist or healthcare professional for a tailored treatment approach.