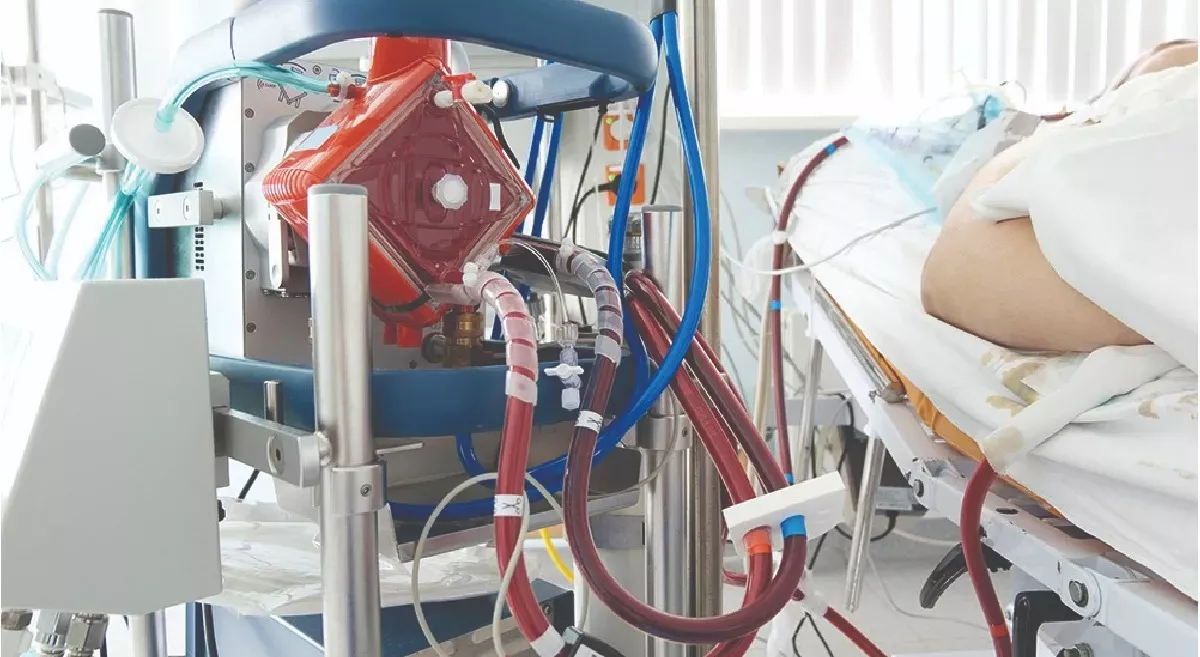
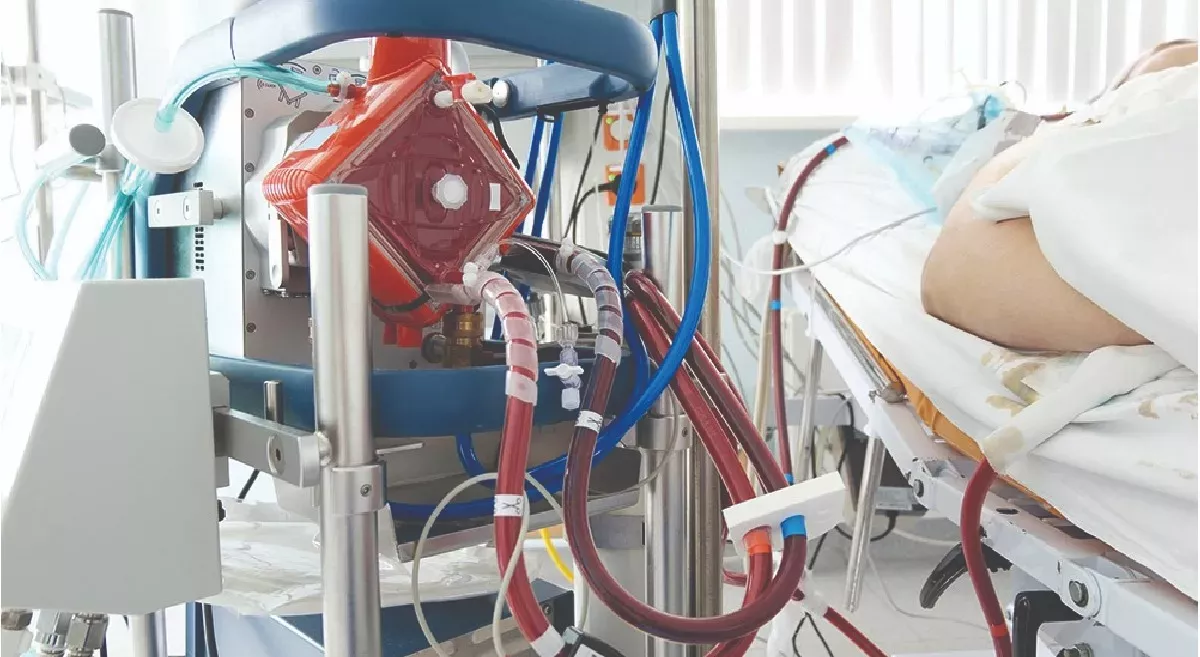
Diffuse alveolar haemorrhage(DAH) secondary to vasculitis usually presents with severe respiratory failure and persistent hypoxia, which is acute in presentation and requires immediate ventilator management . Some of these patients have persistent hypoxia despite conventional mechanical ventilation like lung protective ventilation strategies, recruitment maneuvers, vasodilators, proning protocols. In these patients ECMO can be initiated , because early initiation of ECMO helps in the early phase of the disease helps in adequate gas exchange , hence providing time for the immunosuppressive therapies to act. We hereby present to you a case report of a young female who presented Acute Respiratory Distress Syndrome (ARDS) who was evaluated and diagnosed as DAH secondary to ANCA associated vasculitis , successfully managed with ventilation and early initiation of ECMO. ECMO is not being widely used in DAH given the complications of bleeding. However we managed a strict ACT and APTT during the inititiation and the complete duration of ECMO . We were able to wean the patient of ECMO by Day 5 of initiation without any complications. There are multiple case reports and series recommending the use of ECMO in persistent hypoxia associated with DAH. However before initiating ECMO , complications of bleeding should always be considered and anticoagulants have to be used wisely. We have also reviewed the literature of few case reports and case series and compared the demographic data , complications and outcomes in all these patients initiated on ECMO.
Introduction
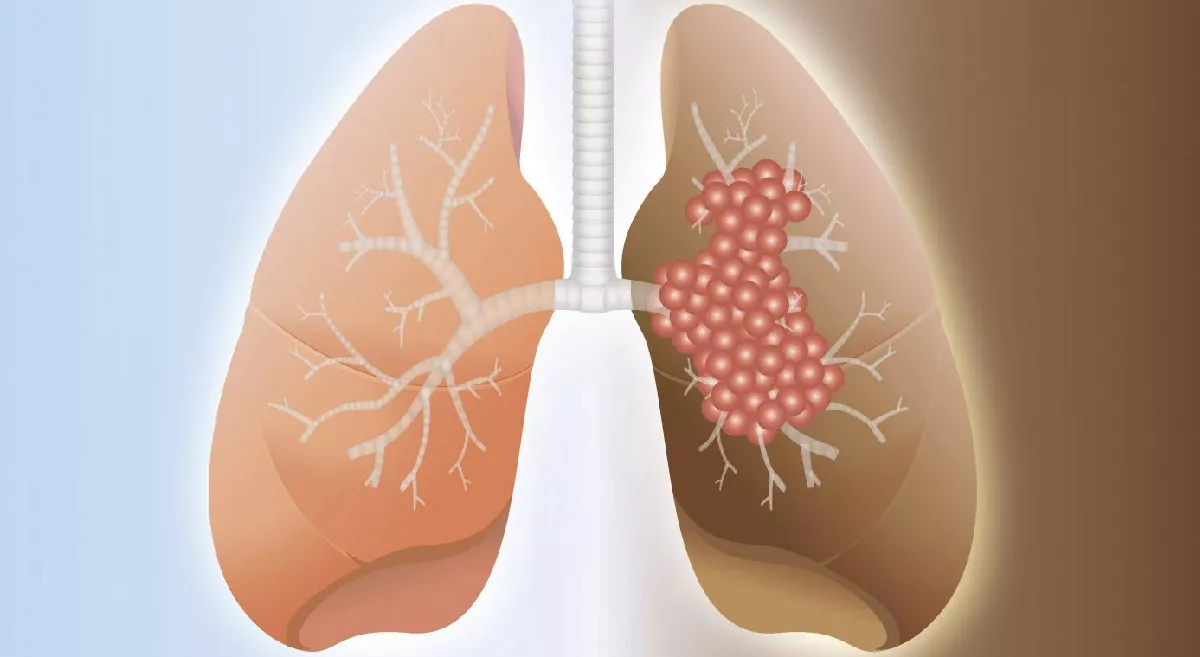
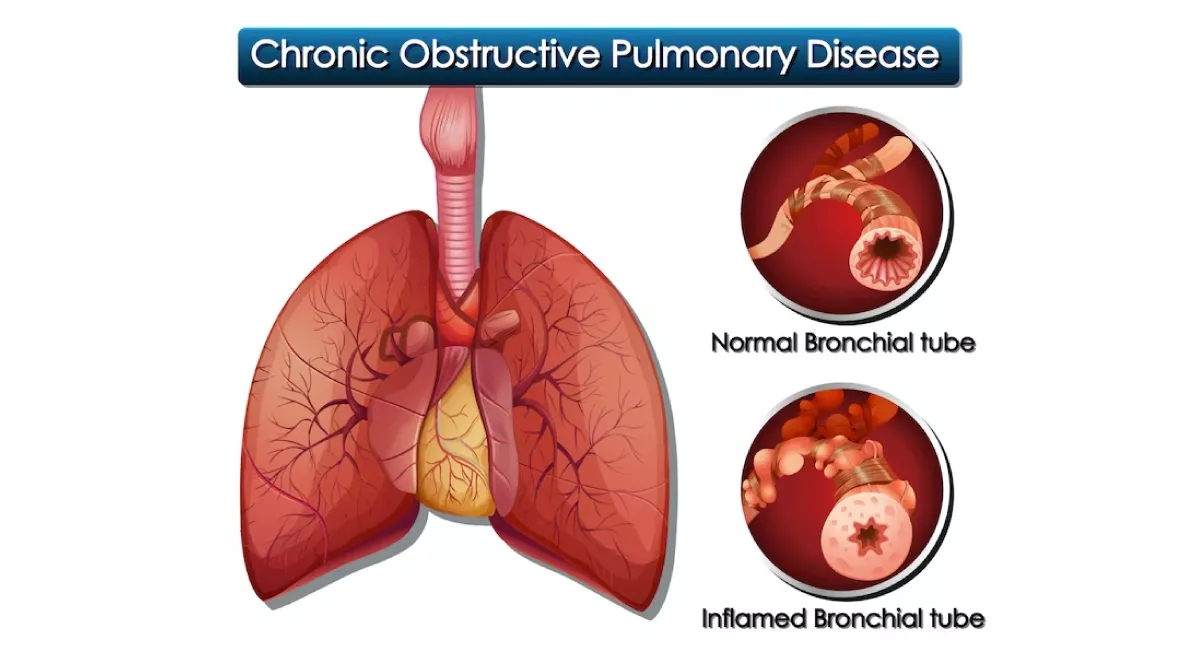
Vasculitis are a group of disorders caused by the inflammation of the blood vessels. Anti Neutrophil Cytoplasmic Antibodies are autoantibodies produced against the antigens present in the cytoplasmic granules of the neutrophils and lysosomes of the monocytes(1,2).Major causes of vasculitis affecting the small and medium vessels of the lungs can be divided into Microscopic polyangitis(MPA), Granulomatosis with Polyangitis (GPA) and Easinophilic Granulomatosis with Polyangitis (EGPA). Vasculitis causes damage to the endothelium thereby disruting the alveolar capillary basement membrane casusing extravasation of the red blood cells to the alveolar spaces .(3)This results in Diffuse Alveolar Haemorrhage(DAH) and sudden respiratory failure requiring the need for urgent mechanical ventilation . Some of these patients continue to be hypoxic even after ventilation , such patients can be initiated on ECMO as early as possible. We hereby present a case of a 27 year old female presented with DAH who was successfully managed with ECMO in Aster RV hospital, Bangalore.
Clinical presentation and evaluation of DAH
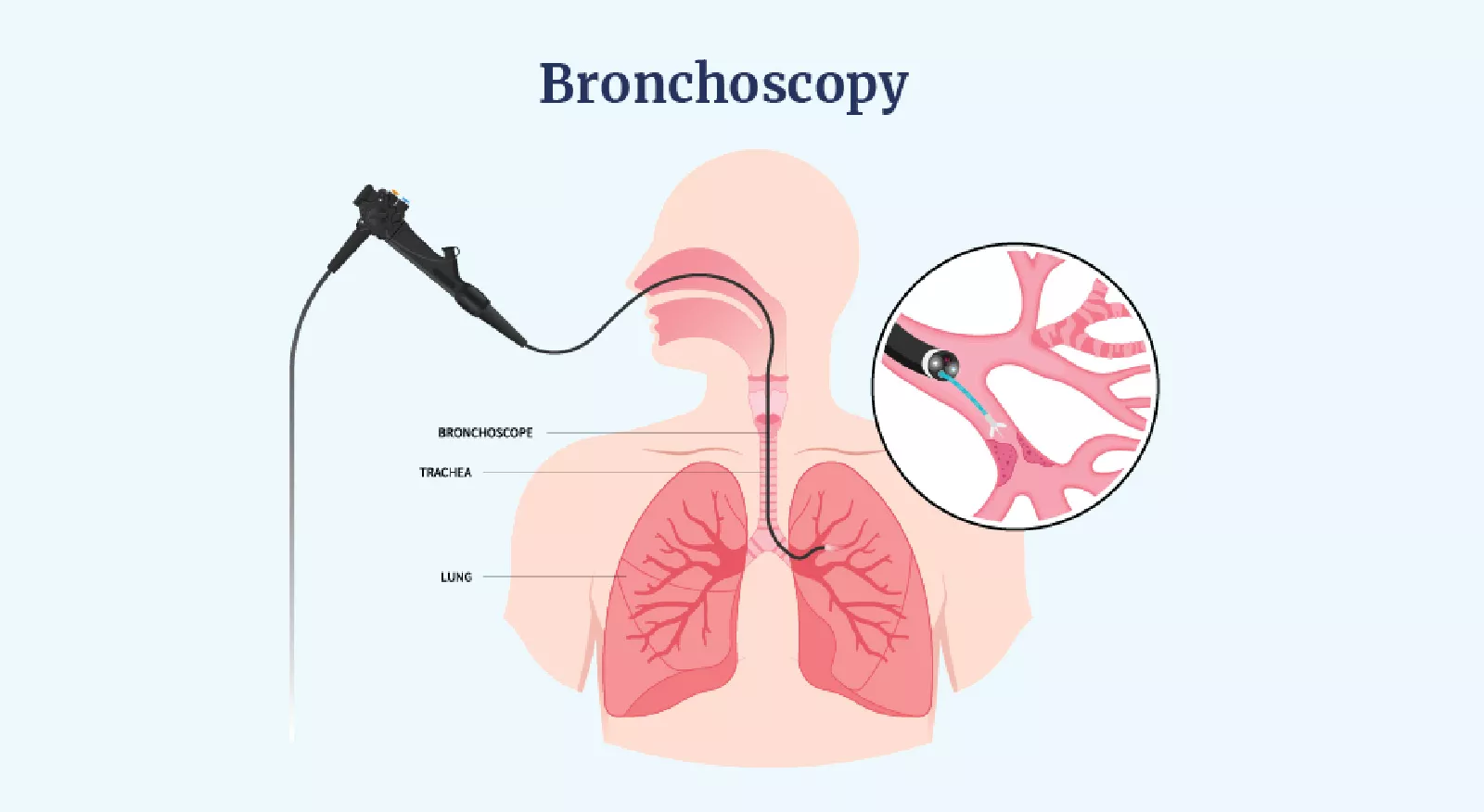
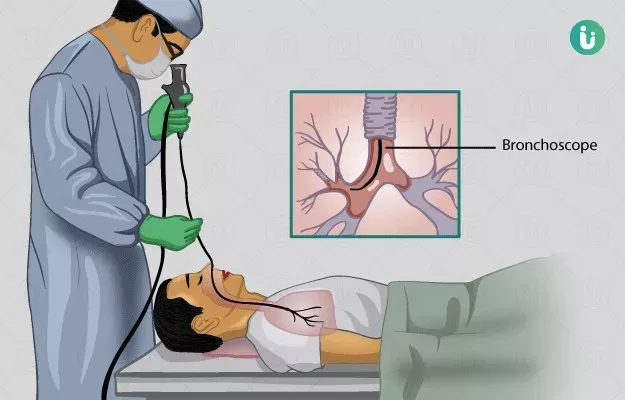
DAH usually presents with fever , haemoptysis , hypoxia , drop in haemoglobin although haemoptysis is present only in one third of the patients . Some patients present with acute onset breathlessness and requiring mechanical ventilation as described in the above case. CT picture shows bilateral ground glassing / consolidation which is diffuse . Recurrent DAH occurs in Idiopathic Pulmonary Hemosiderosis (IPH) resulting in pulmonary fibrosis later. DAH is usually associated with drop in haemoglobin, also since certain conditions are associated with renal damage like glomerulosclerosis, crescentic glomerulonephritis etc , hence associated with the elevation of serum creatinine. The characteristic bronchoscopy picture shows intra bronchial bleeding and sequential progressive haemorrhagic BAL sample. The definitive diagnosis is done by cytology which shows hemosiderin laden macrophages on Prussian blue stain . DLCO will be increased in DAH in stable patients if it can be performed.
Treatment of DAH
Treatment of DAH involves 3 important measures :(15)
Supportive care , haemodynamic stability, vetilatory management with high PEEP , which produces a tamponade effect to reduce the bleeding into the alveoli.
Treat the underlying cause with immunosuprresives , plasmapheresis , antibiotics or antivirals in case of any secondary infections
Rapid and effective local hemostasis .
- DAH in a vasculitis is usually treated with glucocorticoids , pulse iv dose methyl prednisolone (500 to 1000 mg ) for 1-3 days (15) followed by transition to oral tapering doses cam be done. A study was performed comparing the dose effect of corticosteroids for DAH. This study concluded that patients treated with low dose (<250 mg/ day ) corticosteroids had significantly lower ICU mortality rate compared to those treated with medium dose (250-1000 mg/ day ) or high dose (> 1000 mg/ day ), however the overall mortality did not differ(16).We had given similar pulse doses of methylprednisolone. Despite this, patient’s Pao2/ Fio2 was still low and hence was started on cyclophosphamide
- Other treatment options include rituximab, a chimeric monoclonal antibody targeting CD20 has been used . It causes antibody mediated depletion of the CD20 positive plasma cells thereby decreasing the autoantibody production and controlling the disease activity (17,18) .
- Rituximab is given at a dose of 375 mg/m2 per week for 4 weeks as used in the RAVE trial .A study was conducted regarding efficacy and complications of administering rituximab as an induction and /or maintainance therapy in GPA / MPA showed that there is better reversal of the acute illness, however long term therapy resulted in higher rates of infection(19).
- A randomised control trial was conducted comparing the efficacy of combination therapies of glucocorticoids plus rituximab (375 mg/m2once weekly for 4 weeks ) and glucocorticoids plus cyclophosphamide (2 mg/kg/day) showed comparable efficacy of rituximab in remission induction in severe ANCA associated vasculitis , also rituximab showed better efficacy in preventing recurrent renal disease , alveolar haemorrhages(20).
- For achieving hemostasis, Thromboxane A2 can be used intravenous or inhalation form in case of DAH which helps to stabilize the clot inhibiting the conversion of plasminogen to plasmin inhibiting fibrinolysis (21,22,23).
- Cartin Ceba et al (19) conducted a study to evaluate the efficacy of plasma exchange and of rituximab versus cyclophosphamide in patients with DAH secondary to ANCA associated vasculitis with or without respiratory failure. This study was conducted in an institution , where among 73 patients with DAH , 34 of them experienced respiratory failure. This study concluded that no clear benefit in addition of plasma exchange to standard remission induction therapy was seen , however patients receiving rituximab had a higher rate of complete remission by 6 months compared to cyclophosphamide
Conclusion
DAH is an acute life threatening condition which requires timely diagnosis and early initiation of treatment. The case described above was a diagnostic challenge for any pulmonologists given the fulminant course of illness and progressive respiratory failure . This case is a diagnostic challenge for us since the patient was not a previously diagnosed case of vasculitis and this was her first time admission.However timely bronchoscopy , and diagnosis helped us in early diagnosis and ruling out any other associated infections . Also early initiation of ECMO in this patient provided adequate time for immunosuppression induction thereby treating the underlying condition. Hence vigilant work up has to be done in any patient coming with ARDS , keeping in mind rare causes like DAH , because this condition is reversible if diagnosed and treated during the earlier stages of presentation. Also even though ECMO is a highly invasive procedure with increased bleeding risk , it should always be considered in patients with vasculitis associated DAH who has persistent hypoxia post conventional mechanical ventilation. The bleeding risk in ECMO due to administration of anticoagulants and consumption coagulopathy can be managed with vigilant monitoring of ACT/ aPTT .