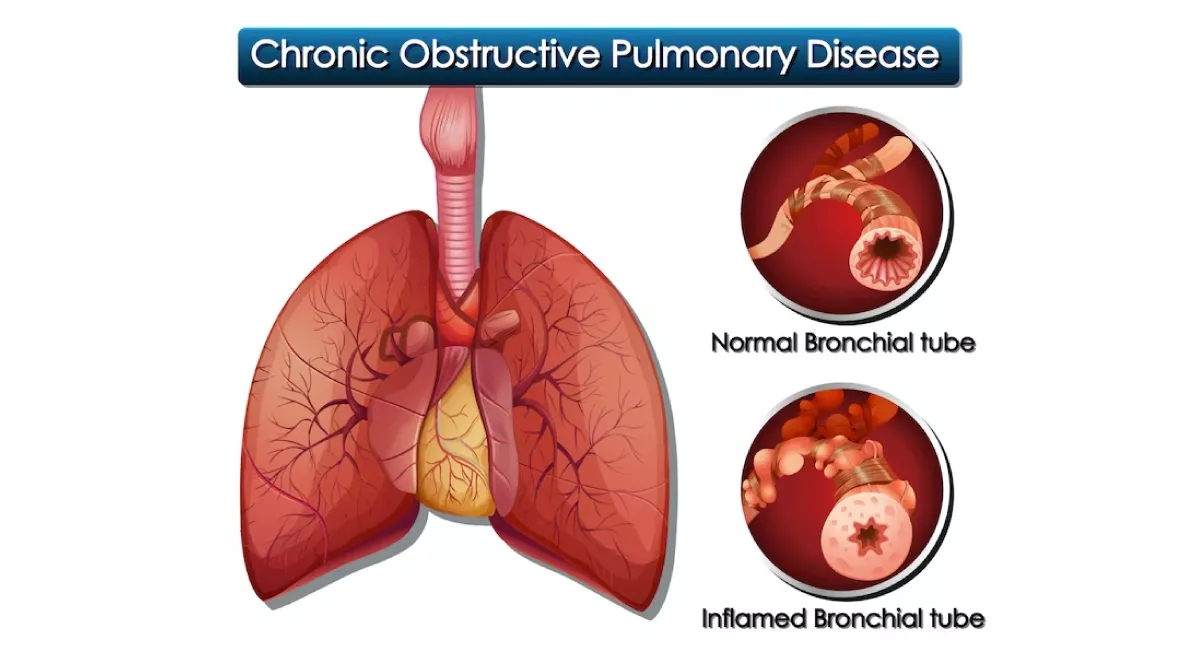
Bronchial asthma, commonly known as just asthma, is a chronic respiratory condition that causes inflammation and narrowing of the airways in the lungs. This can make it difficult to breathe and result in symptoms such as coughing, wheezing, shortness of breath, and chest tightness.
Asthma can be triggered by a variety of factors, including allergens (such as pollen or pet dander), exercise, cold air, stress, and irritants (such as smoke or air pollution). When these triggers cause the airways to become inflamed, the muscles around them may tighten and produce excess mucus, further narrowing the airways and making it even harder to breathe.
There is currently no cure for asthma, but it can be managed with medications (such as bronchodilators and corticosteroids) and by avoiding triggers whenever possible. With proper management, most people with asthma are able to lead active, healthy lives.
How is Asthma diagnosed ?
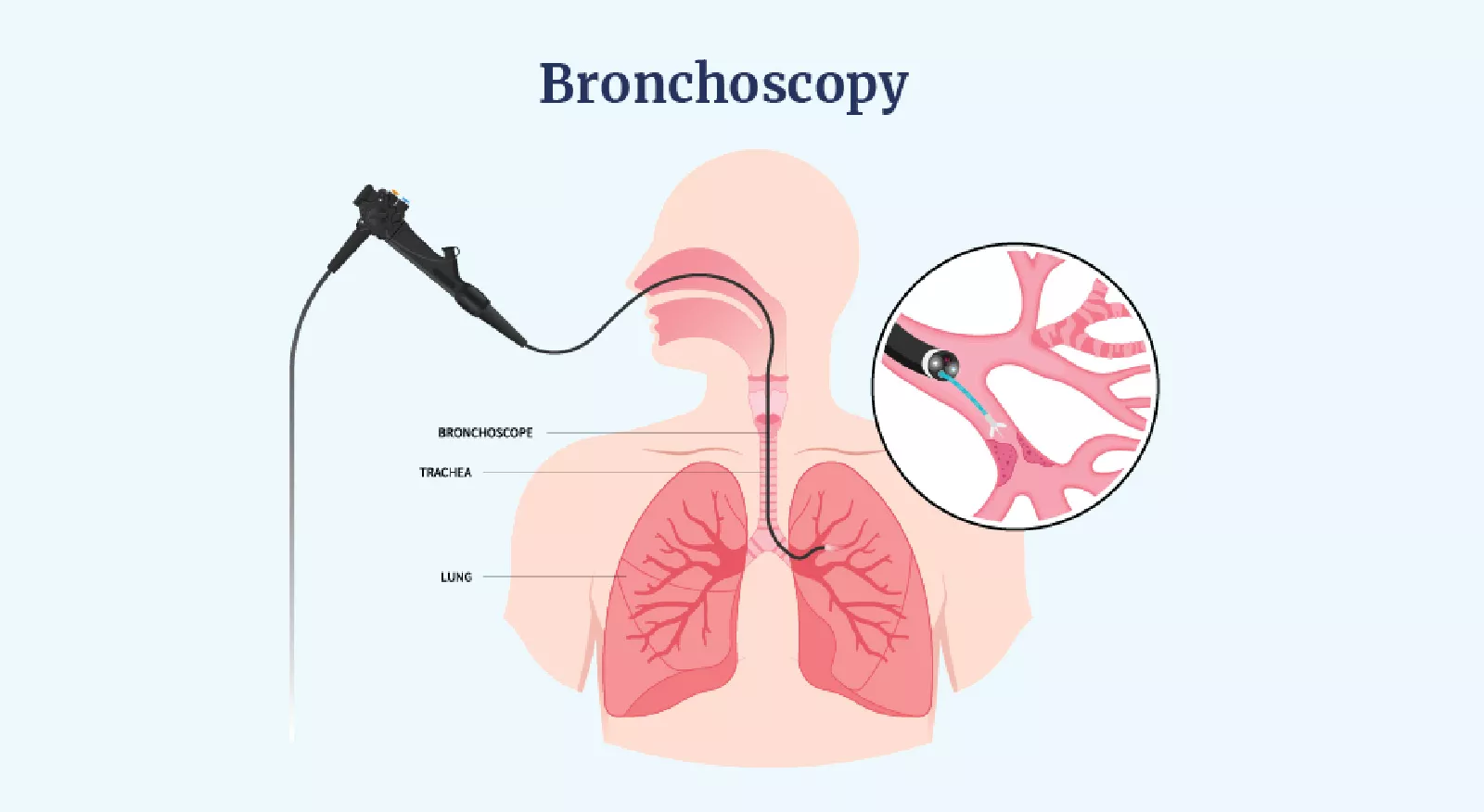
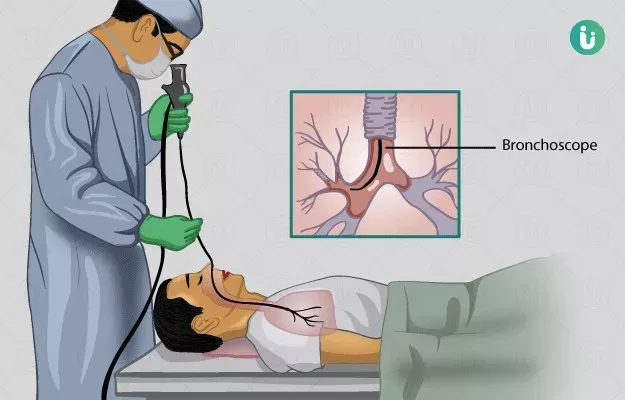
Asthma is usually diagnosed by a doctor or a specialist, such as a pulmonologist. The diagnosis is typically based on a combination of factors, including the patient's medical history, symptoms, physical exam, and lung function tests.
The doctor will usually start by asking about the patient's symptoms, such as coughing, wheezing, shortness of breath, and chest tightness. They will also ask about any triggers that seem to make the symptoms worse. The doctor may perform a physical exam, including listening to the patient's breathing with a stethoscope.
The most important test for diagnosing asthma is called spirometry, which measures how much air the patient can exhale and how quickly they can do it. This test is often done before and after using a bronchodilator medication to see if the medication helps to open up the airways.
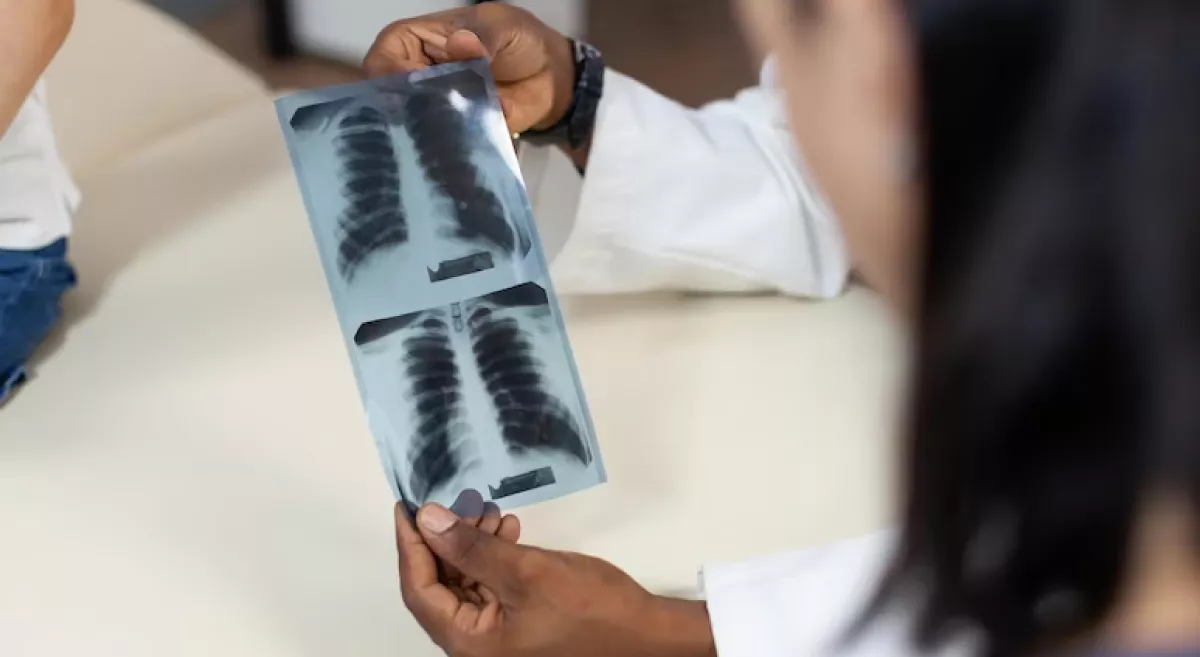
In some cases, the doctor may also order other tests, such as allergy tests or a chest X-ray, to help rule out other conditions that could be causing the patient's symptoms.
It's important to note that asthma can sometimes be difficult to diagnose, particularly in young children who may not be able to perform lung function tests. In some cases, a doctor may need to monitor the patient over time to confirm the diagnosis.
How is Asthma managed medically ?
The medical management of asthma typically involves the use of medications to help control the underlying inflammation and narrowing of the airways. The specific medications prescribed will depend on the severity of the asthma and the individual patient's needs, and treatment may be adjusted over time based on the patient's response.
Here are some of the most common types of medications used to manage asthma:
Inhaled corticosteroids:
These medications are used to reduce inflammation in the airways and prevent asthma symptoms. They are usually taken daily as a long-term control medication.
Long-acting bronchodilators:
These medications are used to relax the muscles around the airways and improve breathing. They are often used in combination with inhaled corticosteroids as a long-term control medication.
Short-acting bronchodilators:
These medications are used to quickly relieve asthma symptoms during an asthma attack.
Leukotriene modifiers:
These medications block the effects of certain chemicals in the body that can cause inflammation and asthma symptoms.
Immunomodulators:
These medications are used in patients with severe asthma who do not respond to other treatments. They work by targeting specific cells or molecules involved in the immune response.
In addition to medication, patients with asthma are also advised to avoid triggers that can make their symptoms worse, such as allergens, irritants, and exercise. Regular monitoring and follow-up with a doctor is also important to ensure that the patient's asthma is well-controlled and to adjust treatment as needed.
What are the precautions to be taken by patients with Asthma ?
Patients with asthma should take certain precautions to help manage their condition and reduce the risk of asthma attacks. Here are some general guidelines:
Avoid triggers:
Patients should identify and avoid triggers that can worsen their asthma symptoms, such as allergens, smoke, air pollution, and exercise. They should also take steps to reduce exposure to indoor allergens like dust mites, pet dander, and mold.
Take medications as prescribed:
Patients should take their asthma medications as prescribed, even when they feel well. Skipping medication or reducing the dose without a doctor's approval can increase the risk of asthma attacks.
Use a peak flow meter:
Patients may be advised to use a peak flow meter at home to measure their lung function and monitor for changes that may indicate worsening asthma. They should report any changes to their doctor right away.
Have an asthma action plan:
Patients should work with their doctor to develop an asthma action plan that outlines what to do in case of an asthma attack or worsening symptoms. The plan may include specific medications to take, when to seek emergency care, and how to manage triggers.
Keep rescue medication on hand:
Patients should keep their short-acting bronchodilator medication (such as albuterol) on hand at all times in case of an asthma attack.
Get vaccinated:
Patients with asthma should get vaccinated against the flu and other respiratory infections to reduce the risk of complications.
Regular follow-up:
Patients should see their doctor regularly for follow-up visits to assess their asthma control and adjust treatment as needed.