Double Lung Transplantation
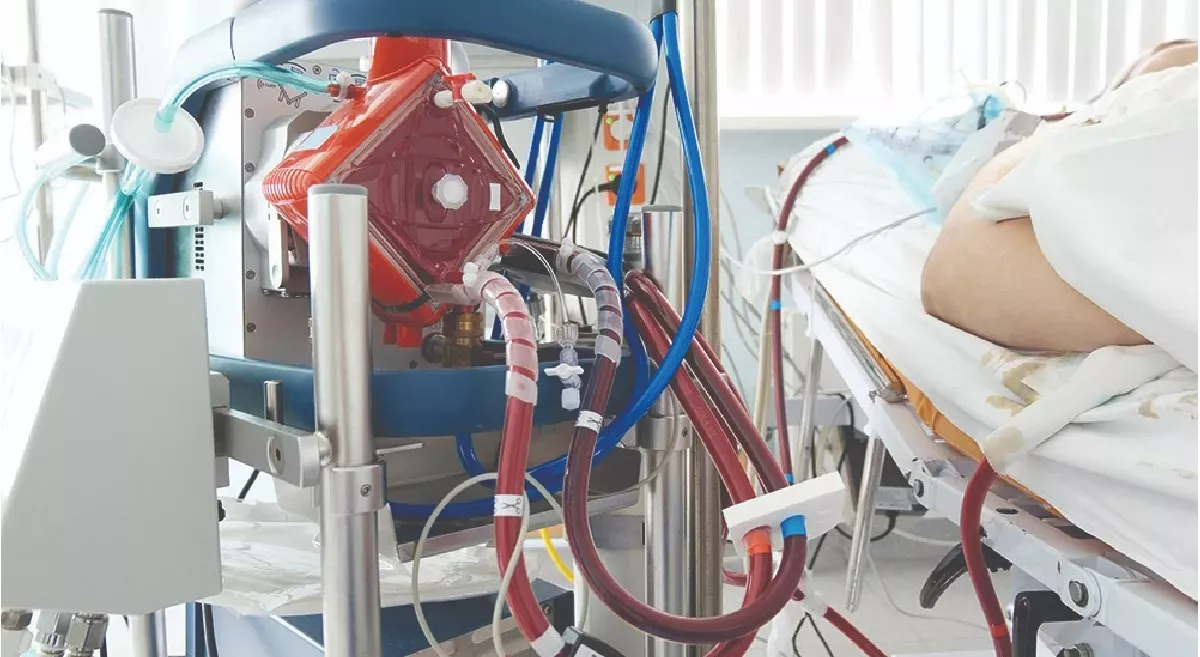
Mr. P a 34-year-old gentleman, was admitted with extensive viral pneumonia, ARDS with lung fibrosis, and Type II respiratory failure. In view extensive lung fibrosis he had to be put on a ventilator support. With further worsening of his lung condition he could not be supported on ventilator alone. Despite being on maximum ventilatory support his oxygen levels could not be maintained. He had to be initiated on another advanced life support called ECMO. Despite receiving Veno-Venous ECMO (VV ECMO)support for a period of 76 days which is one of the longest recorded in India, his lungs did not show any signs of improvement and continued to deteriorate further. After detailed discussions with family and multiple rounds of multi-disciplinary discussions he was considered for lung transplantation.
He underwent a detailed pre transplant evaluation and was found to have blood stream infections possibly from a ECMO cannula site. He was treated adequately with appropriate antibiotics as per culture reports. Repeat cultures were shown to be negative and he was ascertained to be free of infections. He had some critical illness myopathy in view of prolonged ICU stay, limited mobility and he was put on meticulous tailored pulmonary rehab to get him stronger and fit for transplant procedure. Adequate diet was ascertained with enteral and parenteral feeds to maintain good nutrition. After deeming fit for the procedure he was registered for double lung transplantation. After getting a suitable matched donor lungs he underwent a double lung transplantation on 16/12/22 while being on an ECMO support. After the procedure, Mr. P was transferred to the Transplant Intensive Care Unit (TICU), receiving inotropic support, nitric oxide, ECMO, and ventilatory assistance. Inotropic support was gradually tapered off, while enteral nutrition and intravenous fluids were administered to meet his nutritional requirements. The patient was initiated on immunosuppressants, and close monitoring of blood parameters was implemented.
ECMO was gradually weaned off and successfully decannulated on postoperative-day 6 when the newly implanted lungs recovered well and functioning optimally. Over time, Mr. P was gradually weaned off mechanical ventilation and transitioned to oxygen support. Oral feeding was reintroduced gradually, ensuring the patient's nutritional needs were met. Regular evaluations, including echocardiography, chest physiotherapy, and bronchoscopies, were conducted to monitor healing progress and airway stability. Chest tubes were removed as chest X-rays showed improvement.
He was continued on rehab program and was started on mobilisation and oxygen support was slowly weaned off. Following a period of steady clinical improvement and hemodynamic stability, Mr. P was discharged on postoperative day 41 (28/01/23). During follow-up visit surveillance bronchoscopy was normal and lung biopsies were done with no evidence on rejection or infections. CT thorax done was normal and spirometry showed remarkable lung volumes. Today he is totally independent, leading a near normal life, free of any distress and getting back to his professional life. Severe Acute Respiratory Distress Syndrome (ARDS) is a life-threatening condition characterised by profound hypoxemia and respiratory failure.
In cases where conventional therapies such as mechanical ventilation and extracorporeal membrane oxygenation (ECMO) prove inadequate, lung transplantation becomes the only viable option. ECMO is an advanced life support available for sick patients with extensive lung damage. It is used as a bridge until the patient’s lungs recover or in case of no hope of recovery,
ECMO bridge can be used until lung transplantation is done. ECMO can be used as a bridge to recovery from the underlying lung condition or in cases where there is no hope for recovery ECMO is used as a bridge to Lung transplantation.
Dr Gagan (Consultant - Critical Care Unit) explains -
ECMO, which stands for extracorporeal membrane oxygenation, is a lifesupport technique used in critical care medicine. It is a form of advanced life support that provides temporary mechanical circulatory and/or respiratory support to patients with severe heart or lung failure or both. The ECMO system works by removing blood from the patient's body through large cannulas (tubes) placed in major blood vessels. The blood is then pumped through an artificial membrane oxygenator, which functions as an artificial lung, allowing for gas exchange. The oxygenated blood is then returned to the patient's body, bypassing the heart and lungs. There are two main types of ECMO:
What is Venoarterial ECMO (VA-ECMO):
In VA-ECMO, blood is withdrawn from a large vein, typically the femoral vein, and returned to a large artery, such as the femoral artery. This type of ECMO provides both cardiac and respiratory support and is used in cases of severe heart and lung failure.
What is Venovenous ECMO (VV-ECMO):
VV-ECMO involves withdrawing blood from a vein, usually the jugular or femoral vein, and returning it to another vein. This configuration provides respiratory support by bypassing the lungs and oxygenating the blood. VV-ECMO is primarily used in cases of severe respiratory failure, allowing the lungs to rest and recover. ECMO is typically considered when conventional medical therapies have failed to provide adequate support to the failing heart or lungs. It is used as a temporary measure to stabilize patients and provide time for further interventions, such as transplantation or recovery of organ function. ECMO requires specialized equipment, highly skilled healthcare professionals, and close monitoring to ensure proper function and minimize complications. It is commonly utilized in critical care settings, such as intensive care units and specialized ECMO centers, where a multidisciplinary team of experts manages patients on ECMO support. While ECMO can be life-saving, it also carries risks and potential complications, including bleeding, infection, clotting, organ damage, and hemodynamic instability. Close monitoring, meticulous management, and ongoing assessment are essential to optimize patient outcomes while on ECMO support.
Dr. Pavan Yadav Lead Consultant (Interventional Pulmonology & Lung Transplantation - explains the challenges of maintaining a patient on prolonged ECMO -
Maintaining a patient on extracorporeal membrane oxygenation (ECMO) for a prolonged duration presents several challenges due to the complexity and invasiveness of the support. Here are some of the challenges that may arise:
Infection Risk:
Patients on ECMO are at an increased risk of developing infections due to the presence of indwelling lines and cannulas. Infection control measures, including strict aseptic techniques, frequent monitoring, and antimicrobial therapy, need to be implemented to minimize the risk of bloodstream infections and other related complications.
Haemorrhage and Clotting:
ECMO requires the use of anticoagulation therapy to prevent clotting within the circuit. Balancing the need for anticoagulation to maintain circuit patency with the risk of bleeding complications can be challenging. Monitoring coagulation parameters regularly and adjusting anticoagulation therapy based on the patient's condition is crucial.
Vascular Complications:
ECMO involves cannulation of large blood vessels, which can lead to vascular complications such as vessel injury, dissection, or thrombosis. Regular monitoring of the cannula insertion sites and prompt intervention for any signs of complications are necessary.
Mechanical Complications:
The ECMO circuit consists of various mechanical components, including pumps, oxygenators, and tubing. Malfunctions or technical issues with these components can occur and require immediate troubleshooting or replacement to ensure proper ECMO function.
Nutritional Support:
Patients on ECMO often require specialized nutritional support. Feeding through enteral or parenteral routes should be tailored to meet the patient's metabolic needs while considering the limitations imposed by ECMO and associated complications.
Psychological and Emotional Impact:
Prolonged ECMO support can have a significant psychological and emotional impact on patients and their families. The extended hospitalization, uncertainty, and limited mobility can lead to increased stress, anxiety, and depression. Providing psychological support and involving the patient and their support system in decision-making and care planning can help mitigate these challenges.
Rehabilitation and Mobilization:
Prolonged immobilization can lead to muscle weakness, deconditioning, and impaired functional abilities. Initiating early rehabilitation interventions and promoting gradual mobilization when feasible can help minimize these complications and improve overall patient outcomes.
Caregiver Burden and Education:
ECMO support often requires close involvement and coordination with caregivers. Educating and training caregivers about the management of the ECMO circuit, infection prevention, medication administration, and recognizing potential complications are essential to ensure optimal care continuity and patient safety.
Dr.Sandeep Attawar explains the challenges of doing a double lung transplantation in a patient on prolonged ECMO –
Performing a double lung transplantation in a patient on prolonged extracorporeal membrane oxygenation (ECMO) support presents several unique challenges. While the procedure itself is complex, the presence of ECMO adds an additional layer of complexity and consideration. Here are some challenges associated with performing a double lung transplantation in a patient on prolonged ECMO:
Patient Selection: Identifying suitable candidates for double lung transplantation while on prolonged ECMO can be challenging. The underlying condition necessitating ECMO support, such as severe lung disease, must be carefully evaluated to determine if the patient is still a viable candidate for transplantation. The severity and reversibility of the underlying lung disease, overall patient health, and potential risks associated with the transplantation procedure must be thoroughly assessed.
Timing and Coordination:
Coordinating the timing of the double lung transplantation with the patient's prolonged ECMO support can be complex. Finding an appropriate donor match and ensuring the patient is stable enough to undergo the transplantation procedure require close coordination between the transplant team, ECMO specialists, and other healthcare providers involved in the patient's care.
Surgical Considerations:
The presence of ECMO presents surgical challenges during the double lung transplantation procedure. The surgical team must carefully manage the ECMO circuit and cannulas to ensure proper perfusion and oxygenation of the patient during the transplantation process. This requires precise coordination between the surgical and ECMO teams to minimize complications and ensure a successful procedure.
Increased Risk of Complications:
Patients on prolonged ECMO support are at an increased risk of complications during and after double lung transplantation. These can include bleeding due to anticoagulation therapy, infection related to the presence of indwelling lines, graft dysfunction, and rejection episodes. Close monitoring and management of these potential complications are essential to optimize patient outcomes.
Longer Operative Time:
Double lung transplantation in patients on prolonged ECMO may require longer operative times due to the complexity of the procedure and the need to coordinate with the ECMO circuit. Prolonged operative times increase the risk of surgical complications, such as bleeding, infection, and graft-related issues. The surgical team must maintain vigilance and take necessary precautions to mitigate these risks.
Postoperative Management:
The postoperative management of patients undergoing double lung transplantation while on ECMO support is complex. Close monitoring of ECMO parameters, hemodynamics, graft function, and meticulous ECMO weaning process is crucial. Careful coordination between the transplant team, ECMO team, and other healthcare professionals involved in the patient's care is crucial to optimize postoperative outcomes and ensure a smooth transition from ECMO to post-transplant care.
Post-transplant rehabilitation and recovery:
Prolonged ECMO support can lead to muscle weakness, deconditioning, and impaired functional abilities. Rehabilitation and recovery after double lung transplantation in patients on ECMO require a multidisciplinary approach involving physiotherapists, occupational therapists, and respiratory therapists. Gradual mobilization and rehabilitation programs should be tailored to the patient's specific needs and capabilities.
Dr.Prabhat Dutta (Additional Director of Thoracic Organ Transplantation) explains the challenges of a transplant cardiac anaesthetist during a lung transplantation in a patient on prolonged ECMO -
Hemodynamic Instability: Patients on prolonged ECMO often have compromised cardiovascular stability. Anesthetic management aims to maintain hemodynamic stability while minimizing the risk of bleeding and organ injury. Close monitoring of blood pressure, cardiac output, and ECMO parameters is crucial to optimize perfusion.
Coagulopathy and Bleeding Risk:
ECMO can induce a systemic inflammatory response and impair coagulation, leading to a heightened risk of bleeding. Anesthesiologists must be vigilant in monitoring coagulation parameters, such as activated clotting time (ACT) and fibrinogen levels, and be prepared to administer blood products as needed.
Pulmonary Hypertension:
Patients with end-stage lung disease develop pulmonary hypertension, which can be exacerbated during transplantation. Anesthesiologists must be prepared to manage this condition by optimizing fluid status, administering pulmonary vasodilators, and closely monitoring pulmonary pressures with cardiac output monitoring and TEE.
ECMO-Related Complications:
ECMO is associated with various complications, such as cannula malposition, oxygenator dysfunction, clot formation, and air embolism. The anesthesiologist should be familiar with ECMO circuitry and troubleshooting techniques to promptly identify and address these issues.
Acid-Base and Electrolyte Imbalances:
Prolonged ECMO support can result in significant acid-base and electrolyte disturbances, including metabolic alkalosis or acidosis, electrolyte imbalances, and renal dysfunction. Anesthesiologists need to closely monitor these parameters and intervene accordingly.
Anaesthetic Drug Management:
The anaesthesiologist must consider the impact of ECMO on drug pharmacokinetics and adjust anesthesia induction and maintenance accordingly. ECMO can affect drug clearance, distribution, and metabolism, necessitating careful titration of aaaesthetic agents and other medications.
Induction agents – Decision about induction is crucial to select appropriate agent and also weigh the risks of infections vs rejection in a patient on prolonged ECMO.