Symptoms of ILD
- Shortness of breath, especially during physical activity
- Dry cough
- Fatigue
- Chest discomfort or pain
- Unexplained weight loss
- Clubbing of the fingers or toes (enlarged fingertips or toenails).
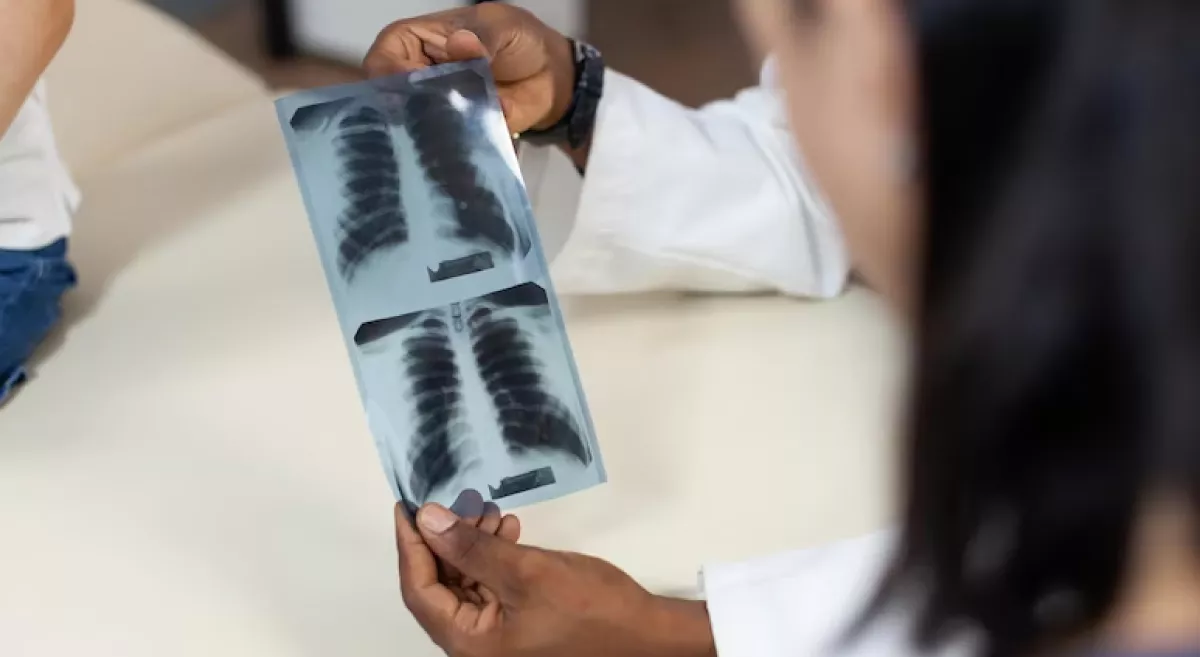
Diagnose of ILD
Doctors typically perform a combination of tests, including:
- Pulmonary function tests to measure lung capacity and how well oxygen passes through the lungs.
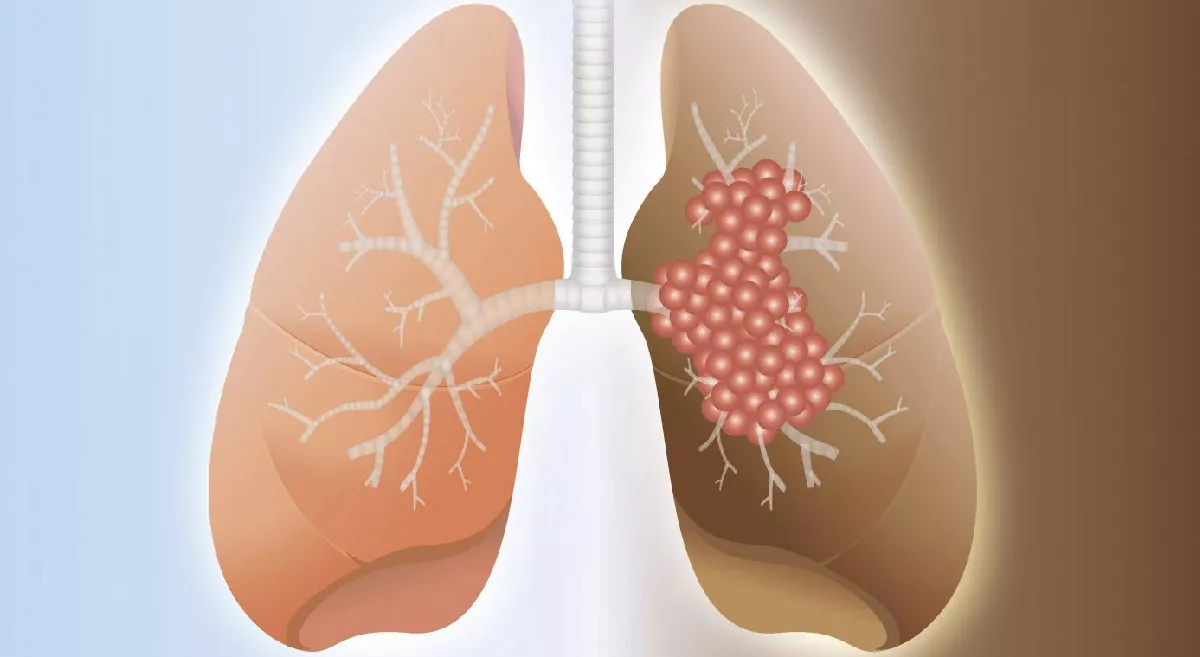
- Chest X-ray or CT scan to check for signs of scarring or inflammation in the lungs.
- Blood tests to check for autoimmune or other conditions that may be causing the symptoms.
In some cases, doctors may perform a lung biopsy to confirm the diagnosis and determine the specific type of ILD.
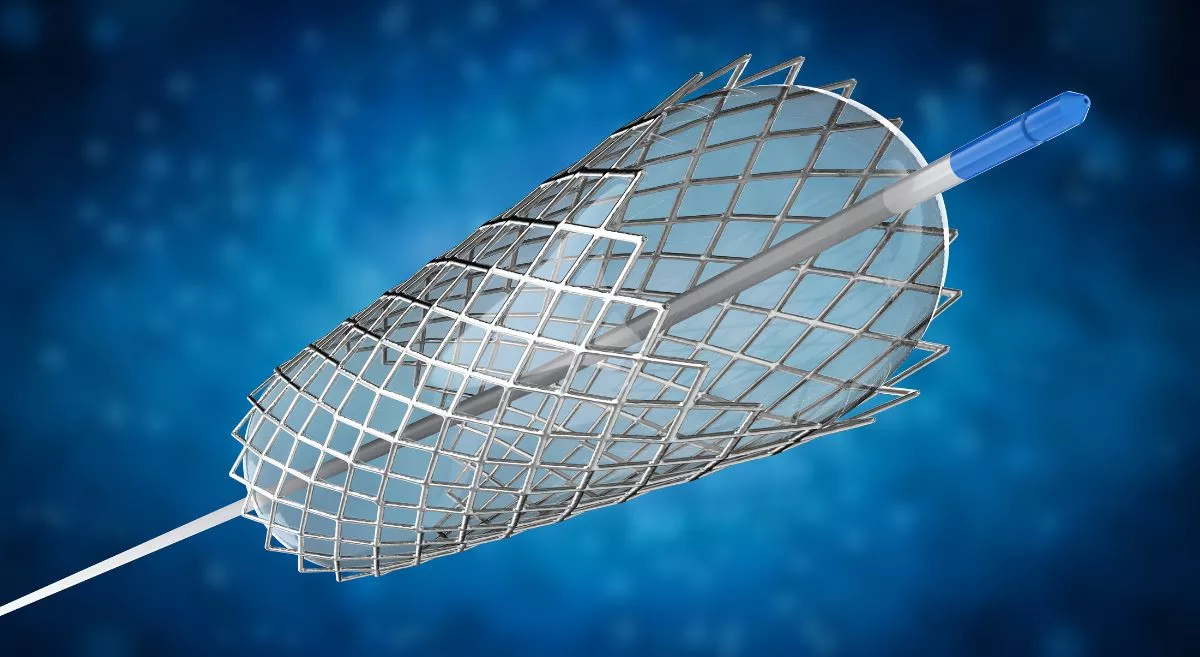
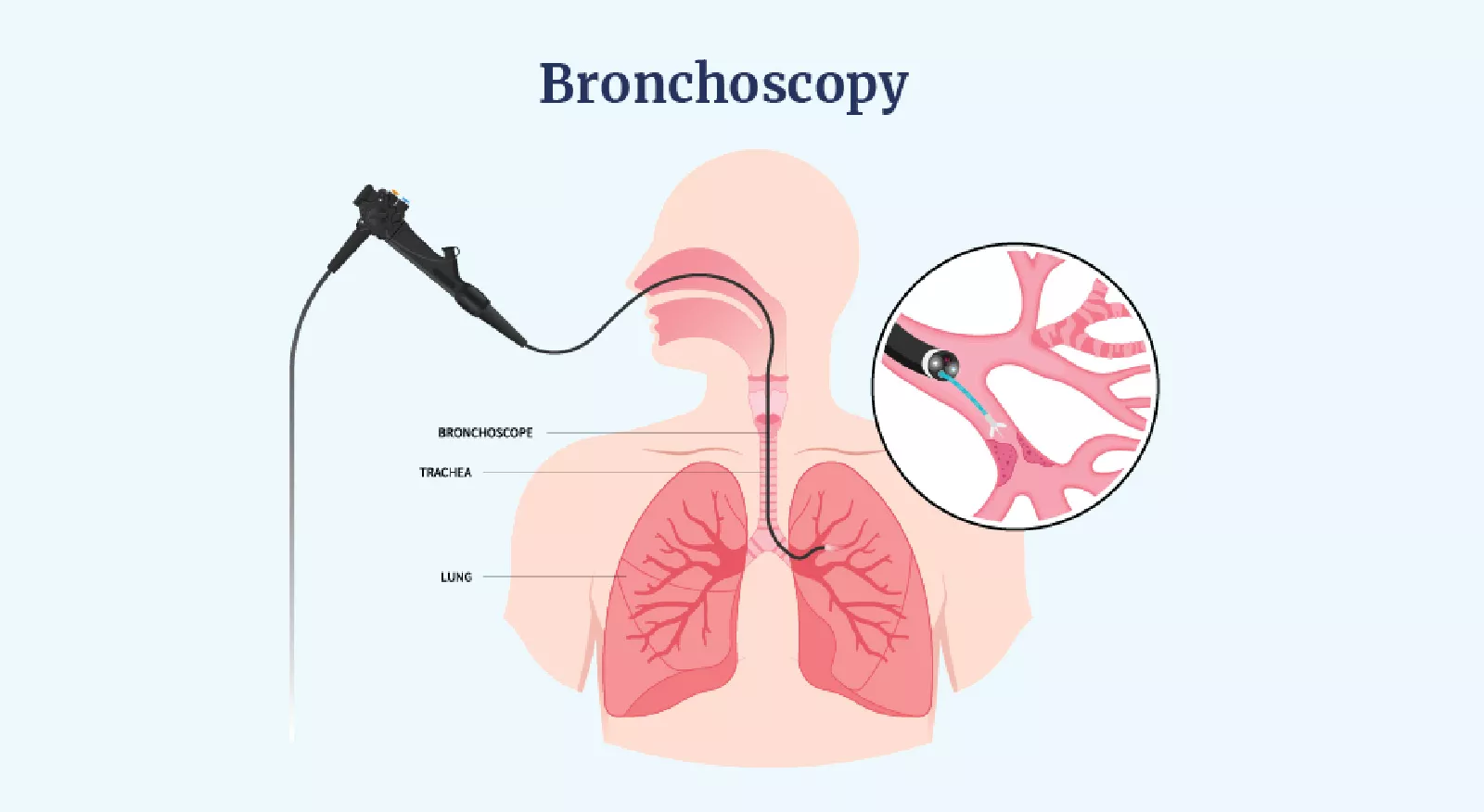
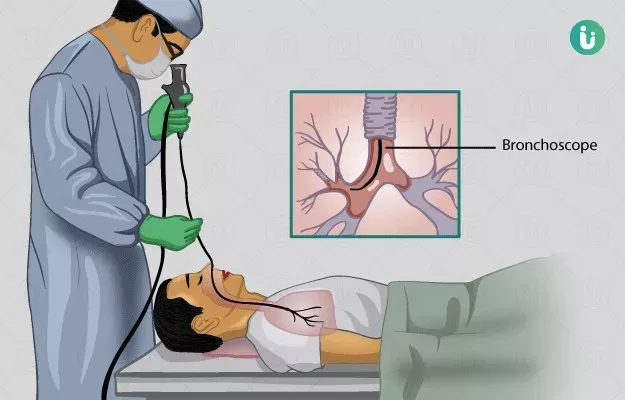
Cryobiopsy of the lungs
It is also known as transbronchial cryobiopsy, is a minimally invasive procedure used to obtain a lung tissue sample for diagnosis of interstitial lung disease (ILD) and other lung conditions.
During the procedure, a flexible bronchoscope is passed through the mouth or nose and into the airways of the lungs. A small instrument, called a cryoprobe, is then passed through the bronchoscope and into the lung tissue. The probe is cooled to a very low temperature, which causes the tissue to freeze and become firm. The probe is then quickly removed, taking a small sample of the lung tissue with it.
The tissue sample obtained through cryobiopsy is typically larger and more representative of the lung tissue than samples obtained through other minimally invasive procedures, such as transbronchial biopsy or bronchoalveolar lavage. This makes cryobiopsy a valuable tool in the diagnosis of ILD and other lung conditions, as it allows for a more accurate and definitive diagnosis.
Cryobiopsy is generally considered a safe and effective procedure, with a low risk of complications such as bleeding or pneumothorax (collapsed lung). However, like any medical procedure, it does carry some risks, and it should only be performed by experienced and trained medical professionals.
Treatment of Interstitial Lung Disease (ILD)
It depends on the underlying cause and severity of the disease. Some treatment options for ILD include:
Medications
Corticosteroids and immunosuppressants are commonly used to reduce inflammation and slow the progression of scarring in the lungs. Other medications, such as antifibrotics, may also be used to treat specific types of ILD.
Oxygen therapy
Supplemental oxygen may be needed to improve breathing and increase oxygen levels in the blood.
Pulmonary rehabilitation
This involves a combination of exercises and breathing techniques to improve lung function, reduce shortness of breath, and increase physical activity.
Lung transplant
In advanced cases of ILD, a lung transplant may be necessary to improve lung function and quality of life.
Treatment of underlying conditions
If ILD is associated with an underlying condition, such as connective tissue disease, treating the underlying condition may help slow or stop the progression of ILD.
Supportive care
This may include measures such as smoking cessation, vaccinations to prevent respiratory infections, and avoidance of exposure to environmental toxins.
It's important to note that the treatment of ILD is typically aimed at slowing the progression of the disease and managing symptoms, as there is currently no cure for most forms of ILD. Treatment options should be discussed with a healthcare provider, who can help develop a personalized treatment plan based on the individual's specific needs and condition.
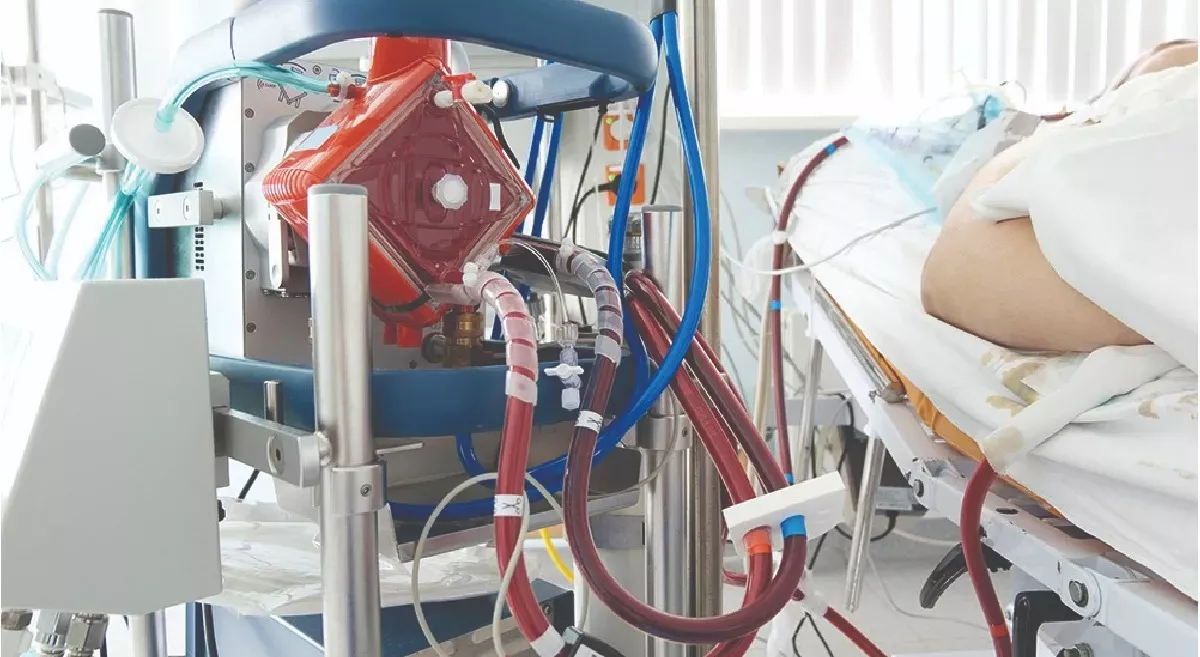
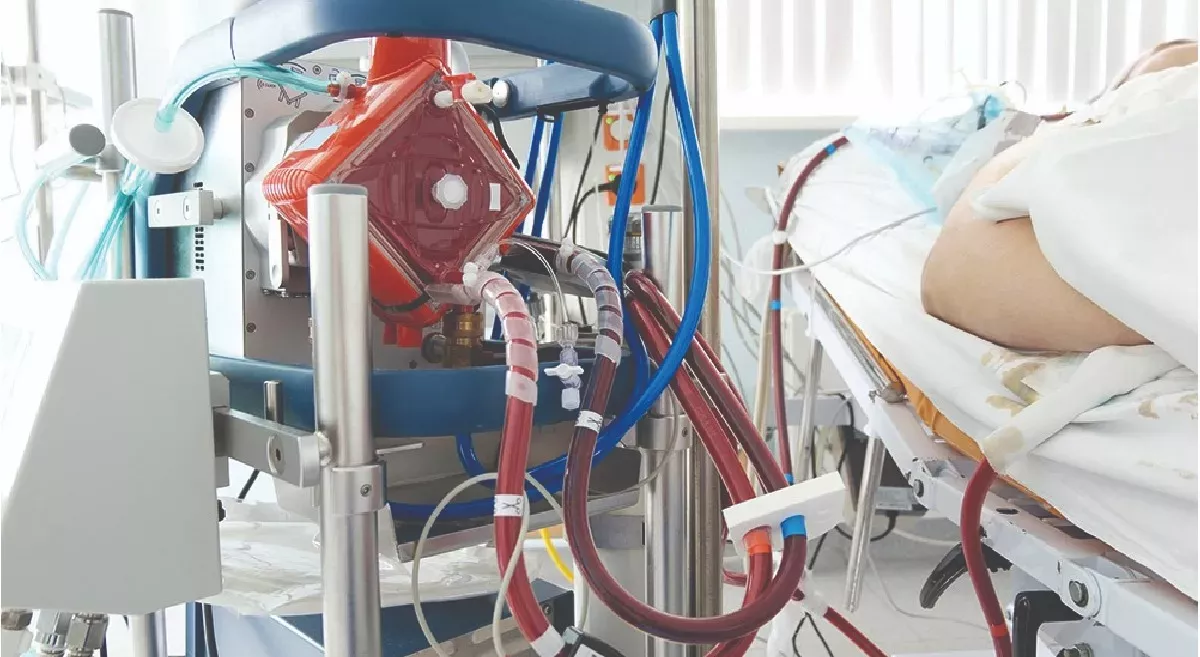
Lung transplantation
Lung transplantation may be considered as a treatment option for people with advanced interstitial lung disease (ILD) who have not responded to other treatments and have a poor prognosis. ILD can lead to severe lung damage and respiratory failure.
Lung transplantation is a complex surgery that involves replacing one or both lungs with a healthy lung or lungs from a donor. The surgery may be performed as a single-lung transplant or a double-lung transplant, depending on the extent of the lung damage.
Before the surgery, a thorough evaluation is conducted to assess the person's overall health and determine whether they are a suitable candidate for transplantation. This may include a medical history review, physical examination, blood tests, pulmonary function tests, imaging tests, and other evaluations.
After the surgery, the person will need to take medications to prevent their immune system from rejecting the transplanted lung or lungs. They will also need to participate in ongoing medical care and monitoring to ensure that the transplant is functioning properly and to manage any potential complications.
While lung transplantation can be a life-saving treatment for people with advanced ILD, it is not appropriate for everyone. The decision to undergo lung transplantation should be made in consultation with a transplant pulmonologist, healthcare provider and based on a thorough evaluation of the person's individual circumstances, risks, and benefits.