A 34 year old female presented to an outside hospital with complaints of high grade fever since 7 days. She was admitted and evaluated at an outside hospital for a week where Dengue, Weil Felix, Leptospira, Typhi dot, Malaria reports were negative. Mantoux and Quantiferon TB gold assay reports were negative. Urine, Blood cultures were negative. CT abdomen done showed mesenteric lymph nodes largest measuring 1.6 x 1.3 with central necrosis in pre vascular region. CT chest showed bilateral pleural effusion. Pleural fluid was tapped and sent for analysis.
Pleural fluid culture grew Pseudomonas stutzeri(? contaminant), which was treated based on the sensitivity pattern. She became clinically better with iv antibiotics and fever subsided for few days. She was discharged on oral antibiotics. However within few days of discharge, patient had recurrent fever episodes which did not subside with antipyretics. She was presented to Aster RV Hospital's emergency department with the above mentioned symptoms.
On examination she was febrile with a temperature of 101F. Her systemic examinations were normal, except for localised left axillary lymphadenopathy. Dengue, Typhoid, Weil-felix were repeated and all were negative. Her blood, urine cultures showed no growth of any pathogenic organism. She had persistent fever which settled only after Naproxen(NSAIDS). Her 2D echo showed normal valves, no foci of any vegetations or valvular abnormalities and normal ejection fraction of 60%.
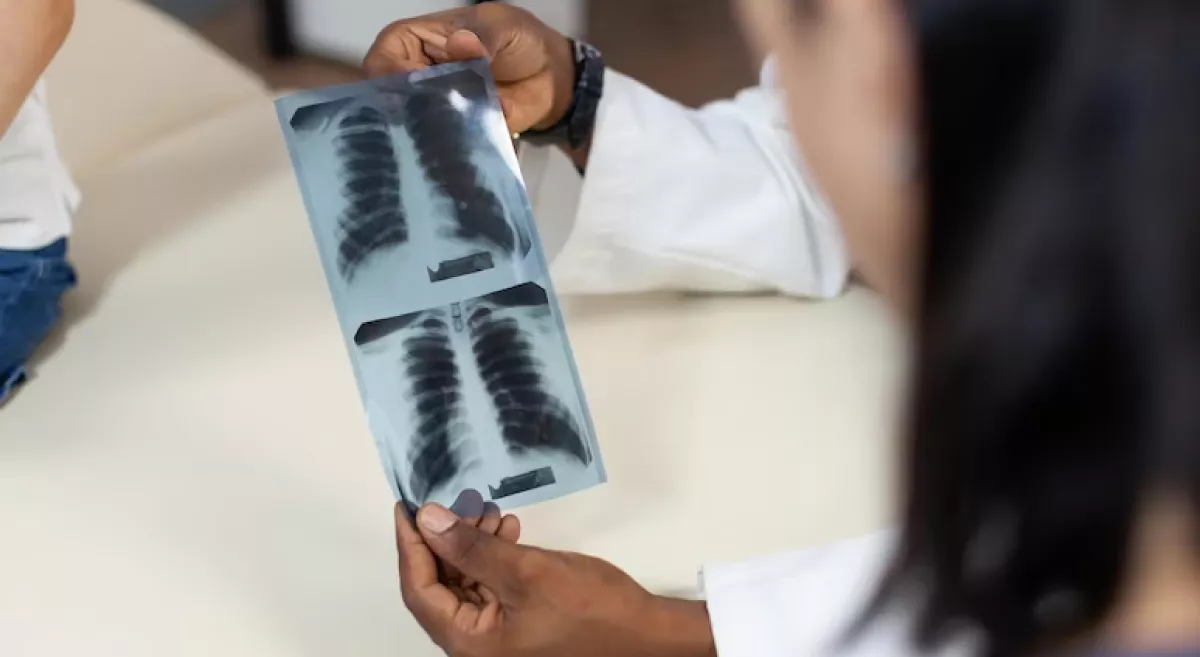
Her CT thorax was done during the admission and showed multiple fibrotic parenchymal bands in the bilateral lower lobes with segmental atelectasis. No consolidation, pleural effusion or ground glass opacity. subcentimeter lymph nodes in the bilateral axillary and right paratracheal regions, measuring 0.8 cm on left and 0.5 cm.
She had developed rashes all over her neck, arms and upper body associated with itching. Hence vasculitis profile was sent, ANCA, RA factor, ANA IF were negative. She was then subjected to PET scan which revealed multiple hypermetabolic lymphnodes on both sides of diaphragm - suggestive of Lymphoproliferative disorder like lymphoma. Histopathologic correlation recommended. The largest and the most metabolically active lymphnode was located in the left axillary node (~ 1.5 cm SUV 7.6) appeared to be the most easily accessible site for a metabolic biopsy.
Post infective/ inflammatory parenchymal fibrotic bands in bilateral lower lobes with segmental atelectasis and adjoining pleural thickening. Since there was a suspicion of lymphoma, Histopathological diagnosis was confirmatory hence, excision biopsy and histopathological examination of the left axillary lymph node was done. The lymph node sample was negative for Gene Xpert MTB, gram stai, negative for aerobic culture and AFB culture.
However on Histopathologica examination showed features of necrotising lymphadenitis with no granulomas, epitheloid cells or evidence of malignancy. The examined lymphnode showed maintained architecture with reactive follicles with sparse neutrophilic infiltrate with crescentic and plasmacytoid histiocytes admixed with karyorrhectic debris.
Differential diagnosis were Kikuchi/ lupus lymphadenitis. Rheumatologist opinion was sought and lupus lymphadenitis was ruled out, as there were no other clinical features of Lupus, and ANA was negative. Hence she was diagnosed to have Kikuchi lymphadenitis and was treated with minimal dose steroids, tapered and stopped. Patient didn’t develop any recurrence of fever/ rashes. She symptomatically improved, afebrile since 3 months and is doing fine now
REVIEW OF LITERATURE
Kikuchi Fujimoto disease or Histiocytic necrotizing lymphadenitis is an idiopathic, self-limiting cause of lymphadenitis.(2) It was first diagnosed in japan in 1972. It was first described to be more common in young females and of Asian descent, however case reports have been described in individuals of African American descent and paediatrics as well.(3)
ETIOLOGY OF KIKUCHI
The cause of Kikuchi lymphadenitis is unknown. However two theories describing infective or autoimmune cause of Kikuchi have been postulated. Viral causes includes EBV, HSV 1,2 , rubella, paramyxovirus, CMV. However none of these viruses have been found in the histopathology of any of these patients. Bacterial causes like Brucella, Yersinia, Mycobacteria species, etc but none of the bacterial cultures grew any of these organisms, hence not proved. However Kikuchi is associated with autoimmune diseases like SLE, Sjogrens, rheumatoid arthritis etc. Given the similar histopathology to autoimmune disorders it is important to exclude autoimmune diseases from Kikuchi by serological analysis. The introduction of IHC, flow cytometry and molecular studies have increased the accuracy of diagnosis. All serological tests like ANA, RA, anti CCP werenegative in our patient, hence auto immune diseases were ruled out.
PATHOPHYSIOLOGY
Kikuchi has been reported to be associated with any physical insults in the body like aseptic meningitis, ILD, post Rouex en Y bypass surgery. It is postulated Kikuchi is more common in certain HLA types in Asian population like HLA DPA1, HLA DPB1. It is as a result of viral or autoimmune cause that would cause this disease. However the exact pathophysiological mechanism is yet unknown.
CLINICAL FEATURES AND DIAGNOSIS
The most common presenting feature is fever and generalized lymphadenopathy usually of the cervical origin, acute in onset and tender. Other symptoms include arthralgia, weight loss, malaise also. However, since all these symptoms are similar to B symptoms in malignant lymphoma, malignancy needs to be excluded by histopathological diagnosis.
Our patient presented with fever, rashes and lymphadenopathy. It has been shown that most of these patients present with leukopenia, increased liver enzymes and ESR. Our patient had an increased ESR, Liver enzymes at the time of presentation (4) Since both tuberculosis and Kikuchi disease presents with necrotising lymphadenitis, Inseon Ryoo, et al (7) had conducted a study comparing the ultrasound features of tuberculosis and Kikuchi disease which showed certain features more common in Kikuchi disease compared to TB. These features include Echogenic hilum, posterior neck involvement, internal necrosis, hilar vascular pattern which are more common in Kikuchi disease than TB.
Ct of the lymph node usually reveals conglomerated lymph nodes, hyper-vascular cortices and necrosis.(8) Given the varied clinical presentation and overlapping features with other systemic diseases like malignancy and autoimmune diseases, histopathological examination and diagnosis is a must.
Our patient underwent an excision biopsy of the axillary lymph node which on histopathological examination revealed Kikuchi lymphadenitis as shown in figure 1. The definitive histopathological picture of Kikuchi lymphadenitis include Karyorrhectic debris, necrosis, crescentic histocytes, Plasmacytoid monocytes.
TREATMENT
Treatment of Kikuchi’s lymphadenitis is only symptomatic. Lymph node tenderness and fever is relieved by NSAIDS. In case of generalized lymphadenopathy and extra nodal disease steroids is the treatment of choice. For steroid resistant and recurrent cases are usually treated with Hydroxychloroquine/ intravenous immunoglobulin(5,6) Kikuchi disease has been reported to recur in 3 to 40% of the population and also recurrence is more common in the paediatric population. The recurrence rate of Kikuchi ranges between 3 and 40%, and recurring disease is more common in children (8.9).
Differential diagnosis
Since Kikuchi is a disease of unknown etiology , It is essential to rule out all the causes that present with similar histological picture as Kikuchi. This includes Tuberculosis , EBV, HSV, rubella , Yersinia infections which can be excluded by molecular tests , smear and culture of the excised tissue. Also autoimmune diseases like SLE, Sjogrens, rheumatoid arthritis , stills disease also present with similar histopathological feature which can be differentiated by doing extensive serological examination.
Also Kikuchi can coexist with connective tissue disease like SLE, Sjogren, Still, hence concomitant diagnosis and management of these disorders is also mandatory. Another differential include lymphoma which also presents with generalized lymphadenopathy. To differentiate lymphoma from Kikuchi disease , peripheral blood smear examination is mandatory which is abnormal in Lymphoma.
On Histopathological examination CD 20 positive B cells are seen in B cell lymphoma, whereas Kikuchi disease shows positive myeloperoxidase staining. Reed Sternberg cells and CD 15/30 positive seen in Hodgkin lymphoma. The above finding helps ne to differentiate Kikuchi disease from lymphoma.
COMPLICATIONS
Kikuchi disease is a rare entity however should always be kept in mind while evaluating a patient for fever of unknown origin. Even though it is a self-limiting disease, complications like Haemhagocytic Lymphohistiocytosis have also been described (HLH). HLH is usually associated with systemic histiocytic proliferation leading to systemic inflammatory response and DIC with a mortality rate of 20 – 42%. HLH is treated with Iv immunoglobulins and Iv methyl prednisolone.
CONCLUSION
With newer diagnostic modalities Kikuchi disease is being diagnosed more frequently. Hence adequate knowledge about this rare entity is essential among clinicians to evaluate, diagnose and treat the same appropriately. PET CT helps in identifying active lesions in the evaluation of PUO and guide targeted biopsies. Timely diagnosis and treatment of this disease is necessary as it is usually selflimiting and life threatening complications are usually rare. Conditions which mimic this clinical conditions including lymphoproliferative disorders, Tuberculosis, metastasis etc should be adequately ruled out.Extensive research is required in the field of etio-pathogenesis of Kikuchi disease as the cause remains still unknown.
REFERENCES
- Petersdorf RG. Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine (Baltimore) 1961;40:1–30.
- Muhammad Masab; Natalya Surmachevska; Hafsa Farooq Jan 2021
- A Case of Kikuchi-Fujimoto Disease in a 7-Year- Old African American Patient: A Case Report and Review of Literature. Am J Case Rep, 2020; 21: e922784
- Zuckerman R, Damiani L, Ayyad HA, Alpert DR. Persistent cervical lymphadenitis in a patient with prior thyroid cancer attributed to Kikuchi-Fujimoto disease. BMJ Case Rep. 2018 Oct 21;2018
- Baenas DF, Diehl FA, Haye Salinas MJ, Riva V, Diller A, Lemos PA. Kikuchi-Fujimoto disease and systemic lupus erythematosus. Int Med Case Rep J. 2016;9:163-7.
- Kim TY, Ha KS, Kim Y, Lee J, Lee K, Lee J. Characteristics of Kikuchi-Fujimoto disease in children compared with adults. Eur J Pediatr. 2014 Jan;173(1):111-6.
- Comparison of Ultrasonographic Findings of Biopsy-Proven Tuberculous Lymphadenitis and Kikuchi Disease. Inseon Ryoo, MD1, Sangil Suh, MD, PhD1, Young Hen Lee, MD2, Hyung Suk Seo, MD2, Hae Young Seol, MD1
- Histiocytic Necrotizing Lymphadenitis Involving the Neck: Radiology-Pathology Correlation Shiraz S. Fidai1 · Nicole A. Cipriani1 · Daniel T. Ginat . Head and Neck Pathology (2019) 13:648–651
- Wang TJ, Yang YH, Lin YT, Chiang BL. Kikuchi-Fujimoto disease in children: clinical features and disease course. J Microbiol Immunol Infect. 2004;37(4):219–224.22.
- 9.Kang HM, Kim JY, Choi EH, Lee HJ, Yun KW, Lee H. Clinical characteristics of severe histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease) in children. J Pediatr. 2016;171:208– 212 e201. doi:10.1016/j.jpeds.2015.12.064
- Kim YM, Lee YJ, Nam SO, Park SE, Kim JY, Lee EY. Hemophagocytic syndrome associated with Kikuchi's disease. J Korean Med Sci. 2003 Aug;18(4):592-4.