PFTs are a series of non-invasive diagnostic tests designed to evaluate the functionality of the respiratory system. These tests provide valuable insights into lung capacity, airflow, gas exchange, and other vital parameters to a pulmonologist, which aids in the diagnosis, monitoring, and management of various pulmonary disorders.
Indications for PFTs
PFTs are indicated in a wide range of clinical scenarios, including:
- Respiratory Symptoms: Patients presenting with symptoms such as dyspnea, cough, wheezing, or chest pain.
- Preoperative Assessment: Evaluating lung function before surgical procedures, especially in cases involving lung resection or transplantation.
- Monitoring Disease Progression: Tracking the course of chronic respiratory conditions like asthma, chronic obstructive pulmonary disease (COPD), and interstitial lung disease (ILD).
- Occupational Screening: Assessing lung health in individuals exposed to occupational lung irritants or allergens.
Usefulness in Diagnosis and Monitoring
PFTs offer several key benefits in the diagnosis and monitoring of respiratory disorders:
- Objective Assessment: PFTs provide quantitative data, enabling an objective assessment of lung function and aiding in accurate diagnosis.
- Differential Diagnosis: PFT results help differentiate between obstructive and restrictive lung diseases, guiding appropriate treatment strategies.
- Treatment Efficacy: PFTs are useful in assessing the effectiveness of therapeutic interventions and guiding treatment adjustments.
- Early Detection: PFTs can detect lung function abnormalities before the onset of significant symptoms, facilitating early intervention.
- Tailored Management: Results from PFTs contribute to personalised treatment plans tailored to the patient's specific needs.
Types of PFTs
Diffusion Capacity of the Lung for Carbon Monoxide (DLCO): DLCO measures the lung's ability to transfer gas from inhaled air to the bloodstream. It is crucial in evaluating conditions affecting gas exchange, such as pulmonary fibrosis and pulmonary vascular diseases.
Oscillometry: Oscillometry assesses lung function by measuring the resistance and reactance of the respiratory system to airflow. This technique is particularly valuable in assessing airway resistance and small airway dysfunction, often seen in asthma.
Fractional Exhaled Nitric Oxide (FeNO) Testing: FeNO testing measures the level of nitric oxide in exhaled breath, reflecting airway inflammation. It aids in the diagnosis and monitoring of eosinophilic airway diseases like asthma.
6 minute walk test: The 6MWT assesses a patient's functional capacity by measuring the distance they can comfortably walk in six minutes. This test is particularly relevant for patients with chronic respiratory conditions, as it provides insights into their exercise capacity and overall cardiopulmonary fitness.
Pulmonary Function Tests (PFTs) serve as invaluable tools in differentiating between obstructive and restrictive lung diseases, aiding in accurate diagnosis and targeted treatment strategies.
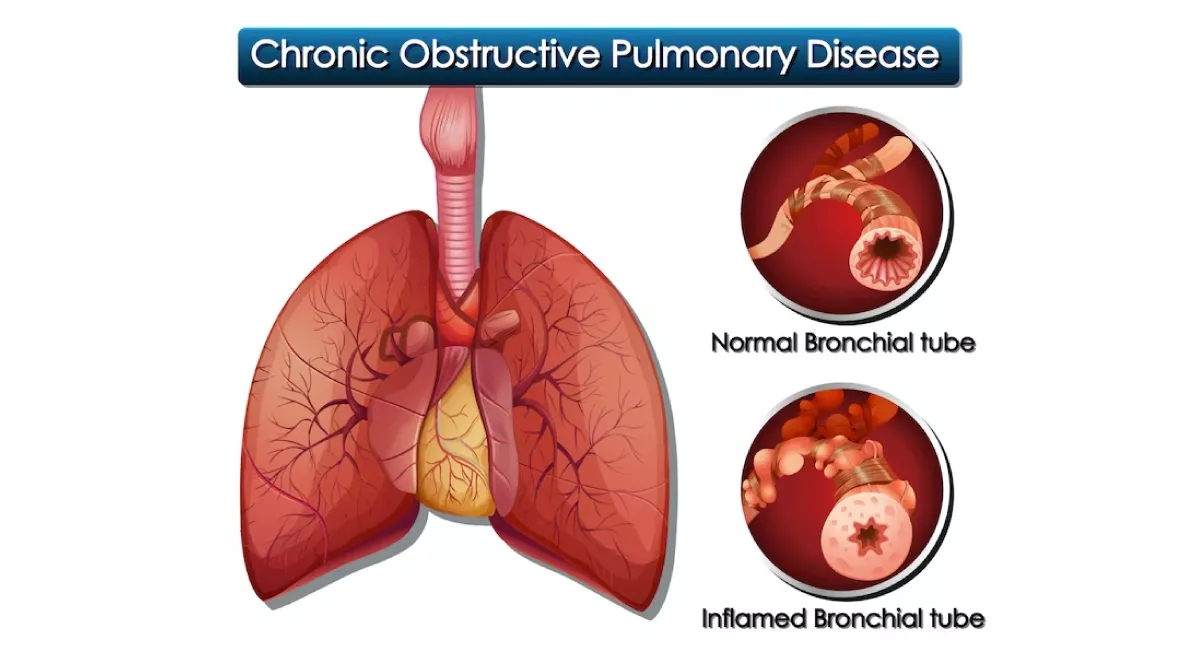
Obstructive Lung Diseases
PFTs play a crucial role in identifying obstructive lung diseases, such as asthma and chronic obstructive pulmonary disease (COPD). In obstructive diseases, the primary issue lies in the airway resistance, leading to difficulty in expelling air from the lungs. Key PFT parameters contributing to this differentiation include:
- Forced Expiratory Volume in 1 Second (FEV1): FEV1 measures the volume of air forcibly exhaled in the first second during a forced expiratory manoeuvre. In obstructive diseases, such as COPD, FEV1 is significantly reduced due to airway narrowing and increased resistance.
- FEV1/FVC Ratio: The ratio of FEV1 to Forced Vital Capacity (FVC) is essential for distinguishing between obstructive and restrictive patterns. In obstructive diseases, this ratio is decreased, reflecting the difficulty in exhaling air quickly.
- Peak Expiratory Flow Rate (PEFR): PEFR measures the maximum speed at which air is exhaled during a forced expiration. Obstructive diseases are characterised by reduced PEFR due to increased airway resistance.
Restrictive Lung Diseases
PFTs are equally crucial in identifying restrictive lung diseases, such as interstitial lung disease (ILD) and chest wall disorders. In these conditions, the lung's ability to expand is limited, leading to reduced lung volume. PFT parameters contributing to this differentiation include:
- FVC: Forced Vital Capacity measures the maximum volume of air that can be forcefully exhaled after a deep inhalation. In restrictive diseases, FVC is reduced due to impaired lung expansion.
- FEV1/FVC Ratio: In restrictive diseases, the FEV1/FVC ratio remains normal or increased, as airway resistance is not the primary issue. The elevated ratio reflects the proportional decrease in both FEV1 and FVC.
- Total Lung Capacity (TLC): TLC represents the total volume of air present in the lungs after maximal inhalation. In restrictive diseases, TLC is decreased due to the reduced lung expansion capacity.
Aster RV Hospital is one of the best pulmonologist hospital in Bangalore, having experienced pulmonologist and advanced technology to provide comprehensive pulmonology treatment.